For this year’s Bowel Cancer Awareness Month, we are supporting Bowel Cancer UK’s #teambowelcancer campaign by showcasing some of the fascinating and vital work that goes on in histopathology laboratories to diagnose this devastating disease.

RCPath trainee member Jade McAlinn is working towards becoming a consultant biomedical scientist in gastrointestinal pathology. She works as an advanced practitioner for Health Services Laboratories and an NHS trainee in gastrointestinal histopathology reporting at the Royal Free Hospital in London.
In a special blog post for Bowel Cancer Awareness Month, Jade talks about her role diagnosing bowel cancer and how she and her team test cases for Lynch syndrome.
Describe your role in the pathology lab – how are you involved in diagnosing and treating bowel cancer?
Any biopsy or tissue removed during surgery to diagnose or treat bowel cancer will be sent to a histopathology laboratory for analysis. One of my roles as an advanced practitioner is to dissect bowel cancer surgical specimens, describing key prognostic features and selecting suitable tissue samples that will be processed overnight in order to prepare a slide.
My training in gastrointestinal histopathology involves looking at the slides under the microscope and writing a draft report. The report will include information such as the type of cancer, its grade, and whether or not the cancer has spread to lymph nodes. In the case of a biopsy, it will include whether or not cancerous tissue is present.
A consultant histopathologist will check the report, amend it if necessary and confirm the diagnosis before sending the results to the clinician. This information is then used to guide treatment and ensure the patient receives the best outcome possible.
How are you involved with testing for Lynch syndrome?
Our laboratory screens all colorectal cancer cases for Lynch syndrome. After diagnosing the tumour under the microscope, a suitable sample area is identified for molecular analysis using a technique called immunohistochemistry. This laboratory technique makes proteins visible which help to identify whether the patient has faulty mismatch repair genes – an indicator of Lynch syndrome.
If the tumour mismatch repair proteins appear normal on microscopic examination, we can confirm that the patient is unlikely to have Lynch syndrome. If the tumour shows loss of expression of one or more of these proteins, the patient may have Lynch syndrome and the tissue is sent to a molecular diagnostics lab for further specialist analysis. The results are added to the histopathology report and sent to the clinician who will notify the patient.
If a diagnosis of Lynch syndrome has been confirmed, genetic counselling can be arranged and the patient and their family will have the opportunity to take steps to help prevent further cancers.
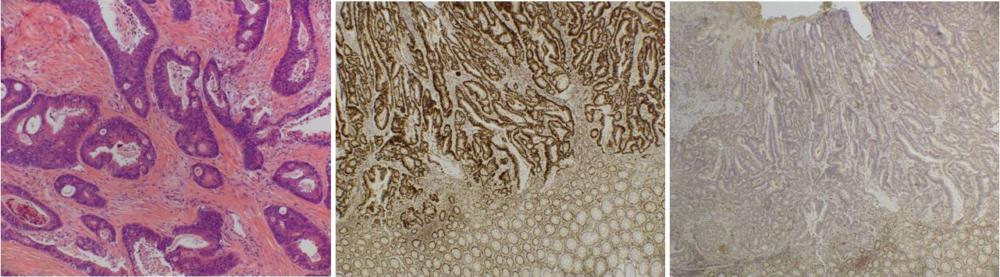
Microscopy images from left:
- Left: Microscopic image of an adenocarcinoma, the most common type of colorectal cancer.
- Middle: Immunohistochemistry for one of the mismatch repair proteins showing normal expression in the tumour. If all four proteins show normal expression, we can confirm that the patient is unlikely to have Lynch syndrome.
- Right: Immunohistochemistry for one of the mismatch repair proteins showing loss of expression in the tumour. This indicates that the patient may have Lynch syndrome and the tissue will be sent to a molecular diagnostics lab for further specialist analysis
Who do you work with at your hospital as part of the healthcare team diagnosing and treating bowel cancer patients?
There is a large and diverse team involved in diagnosing and treating bowel cancer patients. In my own cellular pathology department, I work with biomedical scientists and laboratory assistants to process the tissue, ensure the slides are of good quality and perform specific tests such as immunohistochemistry for Lynch syndrome screening. I also work alongside registrars and clinical fellows, dissecting surgical specimens and learning about microscopic analysis as I progress in my training towards independent reporting.
There are several specialist gastrointestinal consultant histopathologists in our department who are heavily involved in our training and are responsible for the final diagnosis of every patient. The wider healthcare team includes gastroenterologists, endoscopists, surgeons, oncologists, radiologists and nurses.
Every week a consultant histopathologist will meet with members from each of these teams at a multidisciplinary team meeting where every bowel cancer patient is discussed. The outcome is a personalised recommended treatment plan resulting from a collaborative effort between expert healthcare specialists.
Support Bowel Cancer Awareness Month
Around 268,000 people living in the UK today have been diagnosed with bowel cancer. This April during Bowel Cancer Awareness Month, Bowel Cancer UK are running their #teambowelcancer campaign. They’re shining a light on all the people who are there for bowel cancer patients along the way – this includes family, friends, nurses, pathologists, work colleagues, oncologists and more.
The Bowel Cancer UK team invite pathologists and their teams to support their #teambowelcancer campaign. Find out more on their website.

