So, 2020 has certainly been a ‘different’ year for most people, and that is definitely true for us haematologists. Here’s an update about what I’ve experienced, as a general and diagnostic consultant haematologist at Barts Health over the last few months, and what has happened to the department generally.
Changes for me
Before March this year, my working week was a mix of clinics (including a fortnightly trip down the district line to Newham Hospital, deep in the East End), ward rounds, looking down the microscope making blood cancers diagnoses, and lots of meetings at the Royal London Hospital and elsewhere. All that changed when COVID hit, and we all had to make some pretty rapid adjustments to the way we worked and lived.
The first and most striking change was that we stopped almost all face-to-face outpatient haematology reviews. At the height of the crisis, COVID-19 was spreading rapidly. It was not safe for the patients to travel to us and mix in the waiting rooms, and therefore it was only arranged if absolutely necessary. Most of the patients I look after in my subspecialty clinics have benign haematology disease, or chronic blood cancers that only require monitoring or gentle treatments, so all my clinics were, and still are almost exclusively by telephone.
I really miss the personal experience of face to face interactions with my patients, but we’ve been able to provide ongoing vital support to all our patients, in a way which is both time-efficient and in many cases preferable to the patients. We already ran many of our teaching sessions virtually and recorded them for future viewing, to help people avoid unnecessary travel. The vast majority of our meetings are now video calls, which has (hopefully) made us more efficient, and even more people can now access our training sessions.
On the ground in the main hospital, the response and organisation from everyone getting the staff in the right place was nothing short of miraculous. Everyone’s entire work pattern and structure was completely changed, no-one more so than the junior doctors. All our haematology registrars, and many other juniors from lots of specialities became part of the general medical team staffing the COVID ward, leaving the consultants providing all the specialist liaison work, and trying to keep our patients safe at home. We all took on the varied challenges with enthusiasm, but were very grateful for the registrar’s return at the beginning of June when everything started to calm down!

Me back at the multi-header microscope reporting with the registrars (Olga pictured)
After seeing so many patients get so sick with COVID, I was lucky to only be in bed at home for four days over Easter when I contracted the virus, before being back on the wards a week later!
The haematology department also provided some consultants to help cover general medicine, and as someone ‘least departed from general medicine’, I volunteered to help. It had been a while since I last had to think quite so much about non-haematology problems, but it was rewarding to be able to use my skills to help out where I could in a time of crisis. After seeing so many patients get so sick with COVID, I was lucky to only be in bed at home for four days over Easter when I contracted the virus, before being back on the wards a week later!
After that, I hoped my antibodies might be able to help someone with COVID, and willingly volunteered for the national blood service’s exciting plasma trial. I had my run on the plasmapheresis machines that I’ve so often inflicted upon my haematology patients before… but alas, my antibody level was apparently not high enough.

Me at my plasma donation session
Laboratory changes
Although the diagnostic labs and our staff were ready for bone marrow samples, we did notice a drop off in requests, as we know all specialist labs across the country did. Quite rightly, the clinicians and the labs were focused on the COVID patients, whose cases made up the majority of the work during the pandemic. We were seeing some urgent cases, but only hit 30% of our usual diagnostic workload at the peak. The lab staff were still busy, prepping everything to try and improve our service for the subsequent months.
Everything has picked up again now, and it’s largely business as usual for our cancer patients and their doctors, although the lab is now used to working slightly differently. There are lots of measures in place to maintain social distancing, and everyone wears masks all the time.
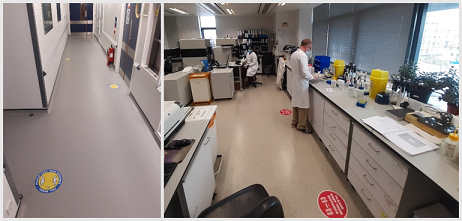
Social distancing in the corridors and scientists Tas and Declan in the immunophenotyping lab.
Where the SIHMDS labs were put into first gear during COVID, the main lab had its extra turbos fitted. Barts Health took on the operational running of the London Nightingale Hospital and we had to set up a brand-new pathology service with good IT links to the new hospital in a matter of days.
We were all ready to be testing samples for 4000 potential patients down the road, on top of a large hospital full of sick patients, and we installed extra machines and changed our work patterns to be ready. Going from testing 100s of coagulation samples a day to 1000s was going to be quite a challenge, and we were ready. Thankfully, the Nightingale Hospital was not needed to full capacity.

Specialist coagulation scientist Sean with one of the new coagulation machines
I really miss the personal experience of face to face interactions with my patients, but we’ve been able to provide ongoing vital support to all our patients, in a way which is both time-efficient and in many cases preferable to the patients.
Overall impressions
COVID has certainly been a challenge for me, and many of my clinical and laboratory colleagues, but I know we’ve had it easy compared to many others, with particular mention for people at the coalface in A&E and ITU. I would also like to mention all those healthcare professionals who sadly died over the pandemic, putting their lives on the line for their patients. I’ve been truly astounded at how well people can pull together in a crisis. I’ve learnt a lot from the experience, including an even greater appreciation for my patients and colleagues, and through switching from public transport to cycling the 44km round journey to work, I may have even got a little fitter in the process!







