Would you like to begin by introducing yourself? What's your role within the service and how long have you been there?
I have been working as a consultant histopathologist at Cambridge University Hospital NHS Trust (CUH) since 2001, specialising in gastrointestinal tract (GI) pathology and cytopathology. I am the lead for diagnostic cytology and upper gastrointestinal cancer pathology services.
My primary research interest is in cancer of the oesophagus and stomach. I am the lead pathologist at Cyted and within an upper GI research team led by Professor Rebecca Fitzgerald, Professor of Cancer Prevention at CUH. Professor Fitzgerald, Marcel Gehrung PhD and I founded Cyted, which is an upper GI diagnostic company that provides centralised data-driven laboratory services for the processing and reporting of CytospongeTM samples.

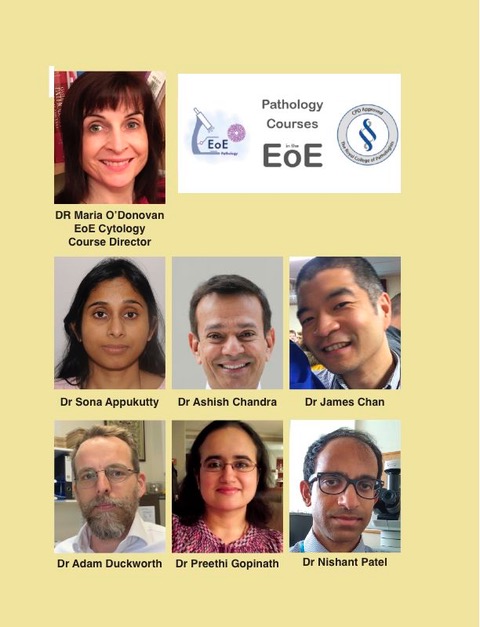
I also get huge professional satisfaction from my role as a teacher. In addition to regular teaching of our CUH trainees, I am a co-director of the not-for-profit East of England (EOE) Histopathology courses, which runs a series of online and in-person histology and cytology webinars for national and international histopathology trainees and consultants. These are RCPath approved for continuing professional development (CPD) points. Many of these courses are FRCPath exam focused. I run and lecture on the cytology courses and workshops.

Could you tell us what sparked your interest in histopathology in the first place?
From early in my medical student training in University College Cork in Ireland I was intrigued by the understanding of disease processes. I had wonderfully enthusiastic pathology teachers, who really helped us understand these changes under the microscope. I was inspired to spend summers, while an undergraduate, assisting in cancer research in the histopathology department. I thoroughly enjoyed this time and elected to specialise in pathology, completing my histopathology training, FRCPath and MD in Dublin before moving to my current post in Cambridge, UK, in 2001.
Could you tell us more about the Cytosponge?
Cytosponge is a device that helps the early detection of the premalignant stage of oesophageal cancer, which is known as Barrett’s oesophagus.
It is a ‘pill on a string’ that contains a compressed sponge within an easily dissolvable capsule. Patients with a history of heart burn or reflux swallow the ‘pill’; the vegetable capsule dissolves in the acid of the stomach releasing the rapidly expanding sponge, which, when being withdrawn via the string, samples the lining cells of the oesophagus. It is a simple, seven-minute procedure, administered by a nurse in a GP or nurse practice setting and is very well tolerated by patients. It has many advantages over endoscopy procedures as a first line test, as it is minimally invasive, cheaper, faster, and can be carried out in primary care settings.
Cytosponge is a device that helps the early detection of the premalignant stage of oesophageal cancer, which is known as Barrett’s oesophagus.
It has been professionally very satisfying to see the Cytosponge device, which I co-invented, make the transition from a research tool to a diagnostic one, being used in daily clinical practice across the NHS. The Cytosponge test has huge potential to revolutionise outcomes, enabling the earlier and faster detection of cancer and supporting pathologists to deliver greater impact, more effectively.

How did your team come to this idea, and which steps you had to take to make it happen? What benefits does it bring to patients and your team?
Firstly, there is a definite clinical need for early diagnosis of this type of cancer. Oesophageal cancer is the sixth commonest cancer worldwide and the UK has the highest incidence in Europe, with adenocarcinoma having increased six-fold since 1990.
Unfortunately, the majority, around two thirds of patients will present with advanced disease, requiring radically drastic surgery and less than 20% of these survive beyond five years. However, with earlier stage disease more than 90% can live more than five years.
There is increased understanding of the molecular alterations involved in oesophageal cancer development. In the UK, most cases arise on a background of change in so called Barrett’s oesophagus (metaplasia) before more increasingly abnormal changes develop (dysplasia) and then cancer.
Firstly, there is a definite clinical need for early diagnosis of this type of cancer. Oesophageal cancer is the sixth commonest cancer worldwide and the UK has the highest incidence in Europe, with adenocarcinoma having increased six-fold since 1990.
Professor Fitzgerald, a clinician scientist, had been working in the field of oesophageal cancer research for a number of years and could see the need for a simple device that could sample the oesophagus to allow the detection of the premalignant phase (Barrett’s oesophagus).
Professor Fitzgerald conceived and designed the Cytosponge device and interacted with industry in it’s manufacture. My role was in developing and optimising the laboratory processes to get the cells from the device, and then moving on to sample processing, slide reading, interpretation and report generation. It has taken many years of hard work from concept to a device that could be used in clinical trials (CE marked, FDA approved) and, ultimately, in diagnostic practice. It has also involved a large team of researchers, doctors, tissue bank staff, nurses, public health staff, bioengineers, bioinformaticians and lawyers, together with collaborators in NHS England and Scotland, general practice and many secondary care gastrointestinal services throughout the UK.

This work has been supported by Cambridge Biomedical Research Centre, Cambridge University, Cancer Research UK, Medical Research Council and NIHR, and has led to numerous publications in high impact journals including Nature Medicine and The Lancet.
In a series of clinical studies involving more than 2,600 Cytosponge procedures across three continents, we have demonstrated applicability to primary and secondary care with excellent safety and acceptability data.
Our most recent trial (13,500 patients) concluded that when Cytosponge was administered to patients with reflux symptoms, ten-times the number of cases of Barrett’s oesophagus were identified, compared to those patients who underwent standard care for their reflux symptoms.
In a series of clinical studies involving more than 2,600 Cytosponge procedures across three continents, we have demonstrated applicability to primary and secondary care with excellent safety and acceptability data.
Cyted UK LTD provides a centralised laboratory service for the processing of Cytosponge samples for clinical users in the UK. The Cyted staff manage all the logistics of delivering a Cytosponge service. All samples are processed at the UKAS-accredited Cyted laboratory, slides are scanned and digitally reported by a team of trained pathologists reporting online from all around the UK. All reported are generated electronically and are readily available for clinical users.
How do you see Cytosponge developing in the future?
I think it would be appropriate for Cytosponge to become a standard test for all UK patients with reflux symptoms, to pick up as early as possible the changes of Barrett’s oesophagus. I can see it having an increasing role in the long-term surveillance of patients with known Barrett’s oesophagus, to help determine the need for endoscopy examination, especially if access to endoscopy is reduced, as happened during COVID-19.
I would also like to see Cytosponge become widely available in the rest of the world, particularly in underdeveloped countries that have a high incidence of oesophageal squamous cancer, where it can also help with early detection.
I would like to see Cytosponge samples examined with larger biomarker panels to molecularly identify the patients at a higher risk of developing oesophageal cancer, as not all patients with Barrett’s will progress to cancer, ultimately incorporating Cytosponge into the treatment/management decision pathways.
I would also like to see Cytosponge become widely available in the rest of the world, particularly in underdeveloped countries that have a high incidence of oesophageal squamous cancer, where it can also help with early detection. We have carried out a feasibility study in Tanzania, Africa.
What role has digital pathology and AI (artificial intelligence) played in your career?
Digital pathology is essential for delivering the Cytosponge service. Glass slides generated from samples are scanned, the online images are read by pathologists in their own homes and reports are delivered electronically to clinical service users. All training for Cytosponge pathologists is performed online. As a result of this we have a large team of pathologists reporting all around the country, allowing for a really quick report.
We are currently developing AI systems to help with the screening of samples. This should aid identification of negative samples and areas within the specimen of interest that will help the reporting pathologists to focus attention and result in a more efficient and speedier reporting process. This will be particularly important in overcoming current workforce issues, enabling pathologists to deliver more impact, more efficiently.
We do anticipate a steadily increasing workload and given the chronic shortage of pathologists in the UK, and this is an important development to consider. This will also have implications in the scaling up of Cytosponge when it hopefully becomes available beyond the UK.
Many delegates told us that they have found our courses invaluable and that there is no way they would have been able to afford to travel to the UK or elsewhere to attend any courses in-person.
Owing to the restrictions imposed by COVID-19, the delivery of our EOE FRCPath courses had to be moved from an in-person course to a hybrid in-person and online course. This has allowed us to reach trainees and pathologists all over the world; participants from Africa, Asia, Middle East, Australia and Europe have all enrolled, with eight trainees from Sudan attending our last course. For our most recent course a number of people from one Pakistani department passed the FRCPath exam, having never been to the UK to attend a course! This was unprecedented.
Many delegates told us that they have found our courses invaluable and that there is no way they would have been able to afford to travel to the UK or elsewhere to attend any courses in-person.
All EQA schemes that I participate in are now digital and this has increased the type of cases that can be discussed. The quality of images and the confidence of my interpretation has also improved with time.
Digital pathology is currently being rolled out at Cambridge University hospital. It will allow the flexibility of reporting from anywhere, home or work which may still be of importance as we learn to live with COVID and its disturbing influence. It also allows for immediate second opinions, without having to send precious slides around the country. Ready access to expert and second opinions, should improve standards of pathology reporting throughout the UK and assist in timely patient management.
How many people are in your teams at Cambridge University Hospitals NHS Foundation Trust? What are their roles and responsibilities?
CUH is a busy teaching hospital with several tertiary and a few national specialties – there is a large array of NHS and NHS/university consultant employees with total subspecialisation. There are monospecialists but with many, like myself, participating in more than one team.
We are an ST1 teaching school and also have a full complement of specialist trainees, academic fellows and specialist neuropathologists and paediatric pathologists.
There is a large histopathology laboratory with designated support for Immunohistochemistry, Tissue bank support for the numerous research projects underway at CUH along with a new molecular pathology department.
Could you describe an average week for you?
On NHS days, I lead the diagnostic and upper GI cancer pathology services, reporting on gastrointestinal and cytology samples, teaching trainee pathologists, giving opinions on tricky or interesting cases to departmental colleagues or on outside referrals, auditing our reporting process and partaking in Upper GI cancer multidisciplinary team meetings.
It’s always interesting to follow up our cases to see if we as a team are getting it right! We can learn so much by knowing the follow up of difficult cases. And it is of real value in the making of teaching cases.
On research days, I look at research samples and help a team of scientists and PhD students answer pathology and research questions on cancer of the oesophagus and stomach.
I also coordinate the online training of Cytosponge pathologists and Cytoscreeners. I provide opinions on difficult Cytosponge cases, as well as input into the laboratory management, development and machine learning teams at Cyted.
There are also items that crop up relating to our EOE course – organising slides for scanning, collecting interesting cases and cataloguing them for teaching collections and courses, as well as coordinating with course speakers and delegates.
It’s always interesting to follow up our cases to see if we as a team are getting it right! We can learn so much by knowing the follow up of difficult cases. And it is of real value in the making of teaching cases.
The beauty of histopathology is that there are always interesting cases appearing on my desk, so I am never bored.
How has COVID-19 affected your work? What steps have you taken to overcome the challenges?
COVID-19 had a massive impact on the endoscopic services across the whole of the UK with very few endoscopic procedures being undertaken, leading to the development of large backlogs of patients with reflux and Barrett’s oesophagus waiting diagnosis and management. This greatly accelerated the setup of the national UK Cytosponge laboratory service.
Reduced staffing levels in the laboratory as a result of COVID illness has made laboratory working conditions more difficult, but I work with teams of great colleagues, and we try to cover the shortfall where possible.
NHS Scotland and NHS England (as part of a trial) adopted Cytosponge to help tackle this problem and the subsequent roll out has made a significant difference to the management of patients and waiting list times.
Reduced staffing levels in the laboratory as a result of COVID illness has made laboratory working conditions more difficult, but I work with teams of great colleagues, and we try to cover the shortfall where possible.
More home and less office working were initially required in the pandemic and this mix has become the new normal for pathologists. Such flexibility has made a significant difference to those of us juggling family and work commitments.
The pandemic made the teaching of trainees much more difficult, as prior to this all day-to-day training was in-person at the microscope. Social distancing requirements made this impossible and it negatively impacted on training. Tutorial sessions were successfully moved online. Although this helped us keep in touch with our trainees it was not always ideal, as the quality of cytology images transmitted from the microscope are often less clear than histopathology images. Thankfully everything is back to normal now apart from all wearing masks (which of course can have their own issues with lots of fogging up of microscopic eyepieces!)
What advice would you give to someone wanting to get more involved in histopathology?
Histopathology is a wonderful career as there are so many areas of medicine in which you can make a difference to patients with diagnosis and prognosis, and also so many research and teaching opportunities. It is also ideal for those who value flexible home working and regular working hours. I have found it particularly conducive to full-time work and family life and have never regretted my decision to follow this career path.
Histopathology is a wonderful career as there are so many areas of medicine in which you can make a difference to patients with diagnosis and prognosis, and also so many research and teaching opportunities.
I would advise anyone thinking of this career to try to spend some time in a histopathology department. Speak to both trainees and consultants, as they can give you valuable advice and insights into the different career stages. Attend multidisciplinary teams and listen to what information the pathologist can give towards patients’ diagnosis and management.
What are you focusing on now as the next step in your career?
I hope to ultimately see a lower incidence in advanced oesophageal cancer during my lifetime, with earlier detection allowing earlier treatment and improved outcomes and ultimately prevention of this horrible disease.
I wish to see Cytosponge being used as a standard diagnostic and screening tool worldwide. To that end I am helping Cyted develop AI systems to accurately read Cytosponge samples, to optimise laboratory systems and to continue training more pathologists to read Cytosponge samples for the UK and beyond.
I hope to ultimately see a lower incidence in advanced oesophageal cancer during my lifetime, with earlier detection allowing earlier treatment and improved outcomes and ultimately prevention of this horrible disease.
I am continuing my involvement in research and focusing on the development of biomarker panels to help identify the patients most at risk of developing oesophageal cancer.
I am also focusing on the continued development and expansion of our EOE histopathology training courses, making sure that we are using all the latest online teaching technology and increasing our collection of workshop cases. I want to continue running these courses to ensure that high standards of histopathology and cytopathology reporting are attained and maintained in the UK and beyond. I want to see more trainees pass the FRCPath exam – we are already seeing a significant improvement in the pass rates of those who take our courses.
Finally, I would like to continue making our courses available to pathologists working in less well-resourced countries.
I have been very fortunate to have had a very varied, interesting, fulfilling and rewarding career so far but none of this could have happened without the support of my wonderful colleagues along the way and of course the ongoing support of friends and family.

