These medals are awarded to pathologists or scientists in training, whose research has the potential to benefit patients and have an impact on the wider pathology field.
In July, we published an interview with Dr Yisu Gu, the winner of the 2024 Gold Research Medal. Now, we are turning the spotlight to our silver medallists.
One of our 2024 Silver Research Medal winners is Dr Jordan Skittrall, who specialises in medical virology and infectious diseases. Dr Skittrall’s winning research focuses on the influenza A virus. We caught up with him to find out more about his background, research and how he sees the field of virology evolving over the next decade.

Congratulations on winning the College's Silver Trainee Research Medal. Please can you tell us a bit about your background? What led you to a career in pathology, and virology in particular?
Thank you! I came to medicine as a graduate entrant. My first degree was in mathematics, and I decided to enter medicine while completing a PhD in theoretical particle physics – so the eventual move to virology was a step up in size from the subatomic particles I had been studying.
I hadn't had any exposure to pathology prior to medical school. I first properly encountered virology during basic science lectures of a traditional preclinical course and found them fascinating. I still remember lectures about viral replication getting me to think very carefully about the ecological niches different viruses sit in... paving the way towards my current studies of evolutionary selection in viruses.
During specialty rotations in clinical school, I realised that not only did I find it immensely fulfilling to help the people who been admitted to the infectious diseases ward, but also that I really enjoyed working on integrating clinical history and examination with diagnostics and treatments, in the deep way that is required in this branch of medicine.
I'd found a group of specialties that fitted the way I like to think about and practise medicine. In pursuing that interest, I was introduced to a group of people who were interested in integrating maths with molecular virology to learn more about human pathogens. I'm grateful to them for getting me caught up in their enthusiasm.
Your winning research covers influenza A genetics. Are you able to summarise this research and what you discovered?
Most of us will have had 'flu’ (influenza) at some point – it's possible to get flu with very few or minor symptoms, right through to serious respiratory illness causing hospitalisation or even death.
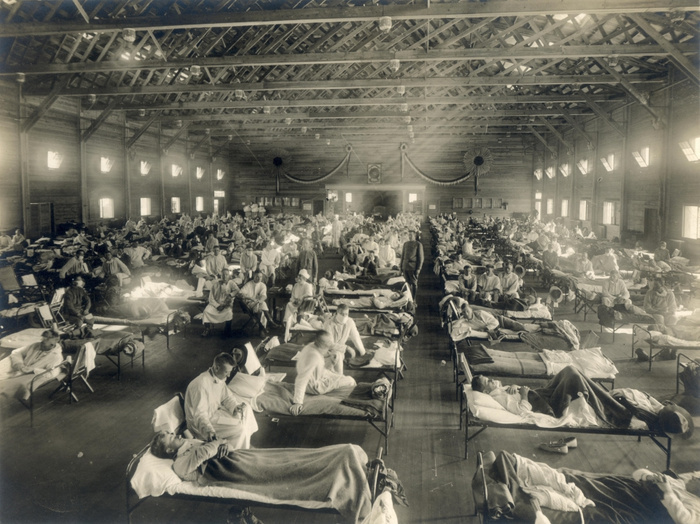
It is estimated that in a typical year, 290,000–650,000 people die worldwide because of influenza, and many more end up in hospital. Furthermore, flu has atypical years. In these years, a new strain of flu emerges to which nobody has good immunity, resulting in a pandemic. There were 3 influenza pandemics in the 20th century, and we have already had one so far this century.
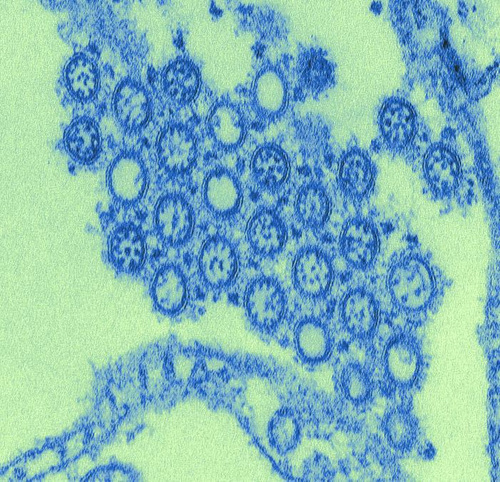
These pandemics happen because there are different strains of the influenza A virus that are better adapted to (and circulate in) different species (e.g. humans, cattle, many birds). The genetic information containing these adaptations is carried on multiple pieces (segments) of genetic material (RNA). Very rarely, when more than one strain of virus infects the same individual host, these segments can get shuffled together (reassorted), resulting in a new virus that is adapted to circulating in humans, but to which humans have not developed immunity. At that point, a pandemic happens.
The research I did, together with summer student Emma Beniston, looked at a number of areas – one of the major areas was how influenza A viruses ‘know’ which genetic material they should be carrying. Each virus particle must make sure it is carrying all the necessary genetic material to make more copies of itself – if not, that will be the end of the line for that particular virus.
So, there is a strong evolutionary driver maintaining the signals that ensure the necessary genetic material gets packaged in the virus particle (we call these signals ‘packaging signals’). This was already known, and previous experiments by others have found approximate genetic regions in influenza A viruses where packaging signals are located. Some experiments have found specific mutations that break packaging, although they have not fully explained why those mutations lead to breakage.
In my previous research, I developed mathematical techniques to find regions in virus genetic sequences where evolutionary selection is at work. In this research, we used those techniques to specify where the crucial genetic regions controlling packaging are, and predicted how the virus's RNA forms structures that act as the recognition signals for packaging.
Our research helps us understand, mechanistically, what is needed at the molecular level for influenza A viruses to be able to package their genetic material. Of course, I am a clinician, and so what I am interested in next is finding ways to break this and thereby help people.

How do you hope this research will influence patient care or clinical practice?
The big goal is to find molecules that will stop this essential part of the virus lifecycle. Because packaging is so critical to the lifecycle, there is a good chance that the virus would find it difficult to mutate to avoid the effects of any molecule we found. Since these packaging signals allow influenza to recognise its own genetic material, the chances of inadvertently targeting something that is essential to us are relatively low. Therefore, if we did find something, there is a good chance of turning it into a useful drug.
I should be clear that we are a long way off that goal – these are only the first steps. Developing any new drug is hard and takes a long time. But the prize, in terms of number of people helped, is worth the effort.
A separate finding from our work is that although the different subtypes of influenza A have recognisably similar packaging signals, there may have enough differences between the corresponding signals, allowing some subtypes to reassort more easily than others. We plan to follow this up because, if that is the case, there will be some virus subtypes that we should monitor more closely for pandemic risk. This would change our approach to epidemiological surveillance.
What impact do you think the COVID-19 pandemic had/continues to have on virology research?
It certainly changed the public profile of virology research. The first years of COVID-19 were the most concentrated public health emergency of the last century. Most virologists switched what they were doing – this certainly led to productive research and clinically useful outputs. However, I would argue the centrality of virology to the response resulted in more disruption to other virology research than it did to research in less-related fields.
Speaking for myself, when COVID-19 hit, I took the decision to intermit the research fellowship I was undertaking to support the initial diagnostic laboratory response. I undertook a lot of COVID-related research – contributing to others' work, and leading my own.
The work I stopped doing was the development of the mathematical theory that underlies the research piece we are talking about today. It resulted in a few years' delay to the flu work. Since I started by using SARS-CoV-2 as the first application of this new theory my collaborators and I developed, I haven’t yet managed to apply the theory to some of the viruses I originally intended to study. This includes dengue virus, which has been estimated to cause around 400 million human infections annually.
What I produced instead has been very useful but different. I am grateful to my very understanding funder.
I think a longer-lasting – and on the world stage currently topical – legacy of the raised profile of virology research has been increased public and political interest and involvement. COVID-19 showed us the value of being able to move research priorities rapidly to respond to emerging challenges, but it also highlighted how one of the strands that supports such flexibility is for research and researchers to have underlying long-term stability. We need to continue to advocate for that – for the sake of good research, and, as clinicians involved in research, for the sake of the patients who have agreed to contribute to research.

How do you see the field of virology, and pathology in general, evolving over the next decade?
Clinical virology has historically found itself facing a chicken-and-egg conundrum between diagnostics and therapeutics: there is no point developing a diagnostic if there is nothing you can do about a problem, and it is difficult to develop a therapeutic for a disease you cannot diagnose in a clinically relevant timescale.
I think many of the innovations with the potential to have the greatest effect in the next 10 years are those relating to near-patient diagnostics. We are now moving into an era where clinical virology has something to say not just about those long-lasting infections that are important to a relatively low number of people, but also about those usually briefer infections that all of us get. Clinically, the challenge in responding to that development is working out how a small specialty – consisting centrally of around 100 consultants practising in specialist centres – can support good use of that information by everybody, in acute care settings in hospitals, and indeed in primary care.
The flipside to developments that push virology out to a greater number of end users is maintaining specialist skill sets in the centre. COVID-19 was remarkable as the first respiratory pandemic where diagnostics continued to be important as the number of cases became very high, and that was mainly because of mass-produced commercial kits that are relatively user-friendly. However, those kits take time to develop, and the very early stage of the pandemic was dominated by specialists developing, validating and using in-house PCRs. As we move more towards mass-produced solutions to meet everyday needs, one of the challenges will be ensuring enough personnel maintain the skills required to respond to the early stages of an emergency.
These developments in clinical virology are a microcosm of what I envisage happening in diagnostic pathology as a whole. The overall narrative is one of greater personalisation in what we can offer. That narrative brings with it the need to make what we offer scale, plus the need throughout that scaling to maintain and develop expertise for the cases that need to be referred.
What is the most rewarding part of your work, and how does it feel to have your research recognised by the College?
I always find this question hardest to answer. The real privilege of my work is the variety. That can be coming up with a new way to understand viruses, or unravelling a part of the virus lifecycle, or unpicking a difficult clinical case, or helping a student really understand something for the first time. The combination of daily ‘wins’ – particularly helping individual patients or students – with contributing to a larger vision gets me up every morning.
I’m really grateful to the College for the recognition. The cross-disciplinary nature of this work means it builds on work from many people, including those I have worked with previously, and benefits from the thoughts and contributions of many others. Despite this, cross-disciplinary work can often feel isolated, and it is really pleasing to receive an indication that the furrow is worth ploughing.
For you, what is the most valuable aspect of being a part of the College, and how do you hope the College will support you and the wider profession in future?
I am at a career stage where most of my contact with the College has been through training and examinations (as a candidate), and I’m now looking forward to engaging with the College from the other side of that relationship.
From a clinical perspective, pathology specialties are often less visible than acute medical specialties – and yet so often provide a critical underpinning to the service we give people. The College plays a key role in supporting good integration of that underpinning function, and I look forward to working with colleagues as we envision what the future of that looks like.
What’s next for you? Are you planning to continue research in this area?
Yes! I’ve recently finished higher specialist training and am transitioning to the next phase of my career. I am keen to continue to integrate research, teaching and clinical practice.
This area of research is sufficiently promising that I want to continue exploring it. Moving from understanding of molecular virology towards therapeutics is multi-step and requires perseverance; seeing on a regular basis the clinical need and potential impact lends a real impetus to action. Like all research, there is no guarantee of success, but influenza is such a large problem that the potential benefits are huge.
We hope that you enjoyed learning more about Dr Skittrall’s research. Keep an eye out for the final interview with our third research medallist, to be published soon.
We are committed to highlighting the incredible work of our members. If you have a story that you want the College to share, please get in touch.

