Would you like to begin by introducing yourself?
Hi, I’m Dr Emily Shaw. I work as a consultant histopathologist in Southampton but also as pathology lead for the new NHS Central and South Genomic Laboratory Hub (GLH). In this role I work very closely with Dr Yvonne Wallis who is a consultant clinical scientist and the lead clinical scientist for cancer at the GLH at Birmingham Women’s & Children’s NHS Foundation Trust.

Hi, I’m Dr Yvonne Wallis and I work as a consultant clinical scientist based at the West Midlands Regional Genetics Laboratory (WMRGL) within the Birmingham Women’s and Children’s Hospital. My role is divided into three parts: co-Deputy Director of the WMRGL (staff of over 250), Head of the Cancer Programme within the WMRGL (comprising both solid cancers and haematological malignancies) and lead solid cancer scientist for the Central and South GLH consortium.

How would you describe what a GLH is?
Dr Shaw and Dr Wallis: The GLHs have been designated as part of a national network of laboratories to deliver increasingly complex and widespread genomic testing as part of the new national Genomic Medicine Service. This testing is performed on blood and tissue samples according to the requirements of the national Genomic Test Directories for rare disease and cancer. This is a massive step forward, since for the first time we have a commissioned and funded service and an agreed ‘menu’ of tests for clinical and laboratory teams, up to and including whole genome sequencing.
The GLHs have been designated as part of a national network of laboratories to deliver increasingly complex and widespread genomic testing as part of the new national Genomic Medicine Service.
What does the Central and South NHS GLH include and when was it established?
Dr Shaw and Dr Wallis: The NHS GLHs were established in 2018 and evolved from the existing regional genetics laboratory structure. As well as the GLH, there is an associated network of local genomic laboratories at other sites in Birmingham, Oxford and Wessex (Southampton and Salisbury).
What challenges have you had to face in the process?
Dr Shaw and Dr Wallis: We both specialise in genomic testing of samples from cancer patients. The demand for this type of analysis has grown massively during the past decade, mainly due to the need to identify patients whose tumours can be shown to bear aberrations that predict response to novel targeted therapies, but also due to the requirement for improved diagnostic classification and prognostic markers. The main challenge is that there is so much to do in meeting the ever-changing demands of this service. The science and technology continues to evolve rapidly, and owing to the organic growth of testing supported from various budgets before the commissioned service, there is an uneven baseline testing activity and access across the healthcare system. We need to try and level up in our efforts to grow the service and ensure equality of access.
Another significant challenge over the 18 months or so has been ensuring the most appropriate technologies are validated and implemented, ready to deliver today’s cancer testing needs but also those of the future. It is critical that we have the capabilities to sensitively detect a breath of genetic variation (including epigenetics) seen in cancer, amenable to both cancer tissue as well as to perform liquid biopsy analysis. The C&S GLH consortium is therefore having to push the boundaries with new genomic technologies, including short and long read sequencing platforms to analyse both DNA and RNA molecules. With increased data comes the need to manage it differently, having to significantly ramp up computing power, bioinformatics pipelines as well as variant interpretation software and reporting to ensure the patient receives as much from the data that we can safely provide at that moment in time.
Is there anything that you think is particularly unique to the Central and South GLH?
Dr Shaw and Dr Wallis: We are the largest GLH region, covering 20% of the population of England, so we have a large number of trusts and clinical teams to engage with and get the message out there that genomic testing is now increasingly available and funded. At the same time, there is significant reconfiguration of teams, processes and workflows going on in all our labs, all within the context of an ongoing pandemic that has affected all of our lives. Specific to this remit, it has contributed to a diversion of staff and equipment to SARS-CoV-2 testing and widespread shortages of vital consumables!
Genomic technology improves efficiency and reduces costs, by consolidating genetic testing to a single analysis. Fast, large-scale, low-cost DNA sequencing also means that it is becoming increasingly available within mainstream medicine, facilitating precision medicine
What do you think is the role and potential of genomic technology in medicine practice nowadays?
Dr Shaw and Dr Wallis: Genomics is an inevitable and exciting transformation of medical practice. The applications we have already seen in terms of making more accurate diagnoses, predicting the course of a disease and response to treatment are still only the tip of the iceberg in terms of what we think can be achieved, and being part of a national service with central oversight and coordination should accelerate progress.
Genomic technology improves efficiency and reduces costs, for example by consolidating multiple genetic testing workflows to a single analysis. Fast, large-scale, low-cost DNA/RNA sequencing also means that it is becoming increasingly available within mainstream medicine, facilitating equitable precision medicine. The increased sensitivity of this technology also means that diseases such as cancer may be detected and then monitored non-invasively, via the liquid biopsy. This one single advancement has the potential to significantly advance the way cancer patients are managed, potentially enabling detection of disease before symptoms present. Earlier diagnosis of cancer as well as earlier detection of relapse increases the chances of successful treatment.
What role does digital technology play?
Dr Shaw and Dr Wallis: Digital technology has a facilitative role in all of this, in terms of tracking, logging and reporting samples. It is also essential for analysis of the increasing amount of genomic data being generated. We have only really just begun to update ageing pathology lab IT systems, implement whole slide imaging, bioinformatics algorithms/decision support for genomic variant filtering and analysis and digital reporting. Within pathology, we are only just scratching the surface of what improvements, insights and efficiencies automated analysis and machine learning/artificial intelligence might bring – watch this space!
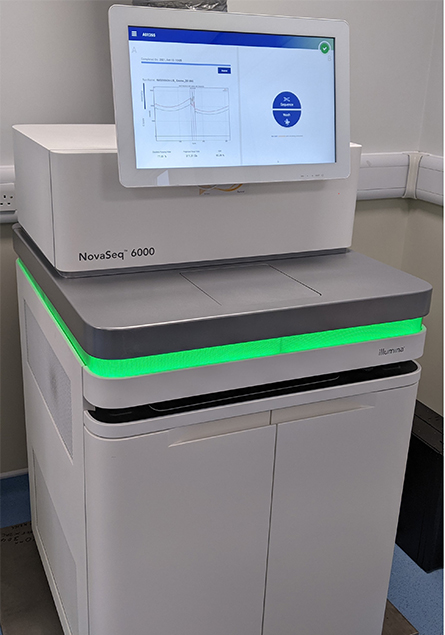
The Nova Seq6000, the latest high throughput sequencing platform which is transforming genomic testing.
What has been one of the most relevant achievements in working with communities and patient groups?
Dr Shaw and Dr Wallis: Genetic testing has clear diagnostic, predictive and treatment benefits. However, it may also be a source of concern for patients and their families, raising issues around privacy, consent, discrimination and equity. The genetics community therefore works very closely with patient groups to ensure these concerns are appropriately listened to and considered. Understanding the ethical issues has been instrumental during the implementation of new genomic tests, such as whole genome sequencing, which is now becoming embedded as standard of care for both rare disease and cancer patients within the NHS. Genetic counselling is essential in discussing ethical issues relating to confidentiality and privacy protection, providing reassurance needed by our patients and their families.
Genetic testing has clear diagnostic, predictive and treatment benefits. However, it may also be a source of concern for patients and their families, raising issues around privacy, consent, discrimination and equity.
How many people are in your team at the WMRGL and what are their roles and responsibilities?
Dr Wallis: More than 250 staff are involved in the delivery of genetic services from the WMRGL with a very diverse skill mix, including clinical scientists, genetic technologists, bioinformaticians, business support, educators, quality managers, informatics and IT specialists.
Within the cancer programme itself, the majority of the 90+ staff are directly responsible for the analysis, interpretation and reporting of genetic data that has been produced from the various genomic technology platforms (DNA sequencing, for example). Again the skill mix is broad, including clinical scientists (registered and in training), as well as genetic technologists and administration support.
For patients with genetic variants in their tumours, it is critical that the technology is sensitive enough to detect them and that the scientists interpret them correctly so that appropriate recommendations can be made to the referring pathology and oncology teams.
The cancer programme at WMRGL is responsible for delivering a huge number of genetic tests within the national Genomics Cancer Test Directory – there are hundreds of tests across adult and paediatric solid cancer and haematological malignancies. Cancer testing involves the analysis of both germline variants (changes people are born with that mean an individual will be at high risk of cancer) as well as genetic changes that have occurred during a patient’s lifetime responsible for cancer development. It is essential that variants are accurately detected (may be just a single change in the background of 3.2 billion normal molecules) to enable the appropriate interpretation and recommendations to be made. If germline changes are detected, for example, then the patient may be at risk of other cancers and their family members will also be at risk of cancer.
By knowing that you carry a cancer variant, better risk-reducing clinical management decisions can be made and tests for family members can be done before the onset of cancer, all with the aim of reducing the development of cancer. For patients with genetic variants in their tumours, it is critical that the technology is sensitive enough to detect them and that the scientists interpret them correctly so that appropriate recommendations can be made to the referring pathology and oncology teams.
Could you describe an average week for you at the WMRGL?
Dr Wallis: This is very difficult as every week is different. We are a very large GLH, serving a population of 12 million people. The range of test requests, technologies and clinical scenarios to process and interpret is huge. As the Head of Cancer Programme my role is to ensure the teams are fully supported in the delivery of the overarching genomic strategy which in itself is constantly changing due to the rapid changes in genomic technology and therefore capabilities. One of my roles is to therefore keep abreast of these changes and strategy and to formulate implementation plans with my teams.
Last week for example I was involved in a number of working groups, one day discussing the clinical utility and roll out of liquid biopsy testing for a broad range of solid cancer patients and then the next day discussing the development of HRD testing in ovarian cancer. Over the next few weeks I will be involved in discussing an emerging long read sequencing technology that may well be introduced over the next few months as part of the cancer testing portfolio. As lead solid cancer scientist for the GLH I work very closely with Emily focussing on the immediate roll out of large cancer panels as equitably as possible across the geography. Whole genome sequencing for cancer patients is also up and running and we are part of a wider team responsible for increasing access to that very complex test.
How has COVID-19 affected your work? What steps have you taken to overcome the challenges?
Dr Wallis: COVID impacted the team and delivery of services enormously in many ways. Social distancing restrictions for example were rapidly introduced in March 2020, and still exist, meaning many of the team are having to work from home regularly. Setting us all up from an IT perspective has been and continues to be a challenge. The physical loss of contact with the team has been a struggle, having to turn to video conferencing as a partial solution, though far from satisfactory.
Wearing masks all day at work is uncomfortable and a challenge for many people especially those with hearing loss, and having to undertake cleaning routines several times a day is disruptive and exhausting. Having said all of that the team pulled together tremendously and continued to deliver services throughout the pandemic. We are starting to see the other side, slowly. Not being able to socialise for 18 months takes its toll. This is starting to happen again. We have a MacMillan coffee morning arranged for next week, which will hopefully offer some light relief as well as an opportunity to try out new cake recipes.
What advice would you give to someone wanting a career in this area?
Dr Wallis: My advice is 'Go for it'. Genomics is a rapidly advancing discipline and its contribution to healthcare is on a steep upwards trajectory. I have been in the field for over 25 years and am still excited by it, by what we are able to do now and by its potential. My PhD was in cancer genetics. I recently worked out that if I was doing it today the technical work would be done in a week, rather than the three years that I spent on it. The progress that has been made in genomics technology has been truly amazing in recent years and the promise to change healthcare is now being realised. So please join the genomics testing revolution – we need you!
Genomics is a rapidly advancing discipline and its contribution to healthcare is on a steep upwards trajectory. I have been in the field for over 25 years and am still excited by it, by what we are able to do now and by its potential.
What are the challenges for the Central and South GLH consortium in the future and what are you looking forward to?
Dr Wallis: Yes very much looking forward to the future of the Central and South GLH consortium. We work with a fantastic team across the whole geography, all of whom are committed to the delivery of the highest quality genomics services. I feel privileged to be part of the team.
Of course, there are going to be challenges, including as always funding to ensure the best genomic tests can be delivered to all patients that need them.Workforce will also be a challenge, ensuring we can recruit and retain the numbers of appropriately qualified personnel that are needed for this rapidly growing service. IT is a barrier to rapid implementation of high throughput testing, analysis and reporting, which requires efficient connectivity, analytical power and data storage. Another challenge will be how to use the huge amounts of genetic data that is going to be created safely for research, for example to support recruitment to clinical trials. Saying all of that, we have overcome so many challenges in the last three years that I have no doubt that we will overcome all of these to be part of a truly transformative genomics network.

