Would you like to begin by introducing yourself? What's your role within the service and how long have you been there?
Hi, my name is Maggie Morgan and I work at Health Services Laboratories (Sonic Healthcare UK) in central London. I am a Consultant Biomedical Scientist and Head of Cervical Screening Service. I first joined the company in 2011 and have been involved in a progressive large-scale centralisation of cervical screening services in London. In 2019, Human Papilloma Virus (HPV) molecular testing replaced cytology as the frontline test for the detection of pre-cancerous changes of the cervix. Using molecular platforms for testing has opened the doorway for large scale automation and a move away from more traditional manual techniques.

Could you introduce us to your team – how many people are in the team and what are their job roles?
The cervical screening team comprises close to 90 staff made up of laboratory support workers, administration assistants, biomedical scientists/cyto-screeners, managers and a clinical team of 20 consultants.
Everyone employed within the service works to deliver cervical screening for London. Over 700,000 samples are delivered to the flagship Halo building in central London by a dedicated courier fleet.
Samples are received and requested onto the pathology system and histories checked against the national cervical screening database.
Samples are then tested for HPV using an RNA based assay which detects integrated HPV virus. Reflex cytology is carried out on HPV positive samples. A positive HPV test with abnormal cells identified on cytology will require individuals to be referred to colposcopy for assessment of the cervix and further investigation/treatment if required.
Other key aspects of the service include participating in multi-disciplinary team meetings (MDTs) with colleagues from 26 colposcopy units across London. MDTs are pivotal to ensure individuals receive the best care. In the new world, MDTs are successfully delivered. Cytology, histology and colposcopic images of the cervix can all be shown using virtual video conferencing linked to microscopes back at the central laboratory.

Is there anything that you think is particularly unique to your team at the Health Service Laboratories in London?
Yes, indeed. The current workforce has been brought together into one unit from across NHS Trusts who previously carried out cervical screening in smaller hospital-based laboratories. The team is made up of dedicated professionals who are fully committed to providing a screening service for London. It is not easy merging workforces, but their dedication to the service throughout the pandemic has been commendable. The new service moved into the Halo building on Thursday 19th March 2020 and lockdown followed within days on 23rd March 2020. Despite the challenges, the team continued to deliver a first-class service.
What role does digital technology play in your experience and how do you see this developing in the near future?
Radiology and pathology have been embracing digital technology for some time, with cytology falling behind partly due to lack of technological innovation. Cytology cells are more three dimensional, unlike histology sections. Once digital systems have been adequately developed, the next steps would be addressing challenges around IT, storage of colossal data files, testing and, of course, user acceptance with, hopefully at some point, integration into the NHS screening programme.
Digital cytology systems are not in routine use but have the potential to offer an alternative approach to cervical screening.
Digital cytology systems are not in routine use but have the potential to offer an alternative approach to cervical screening. Glass slides will be scanned and images presented to the cytologist on a high resolution monitor for interpretation.

What has been one of the most relevant achievements in working with communities and patient groups?
Cervical Screening London (CSL) was proud to receive an Achievement Award from the RCPath for its contribution to speciality in 2020. We are continually working to deliver service improvements.
At CSL, we are also particularly proud of our Sample Taker Bulletin – a quarterly communication to all sample takers in London. The bulletin is cascaded by the National Health Service England (NHSE) and the Integrated care systems (ICS) networks. A new approach is to invite professionals involved in cervical screening to contribute to the bulletin. The South East London Cancer Alliance and RM Partners.
Could you describe an average week for you and your team?
A cervical screening laboratory is dynamic, diverse and complex. I would encourage professionals involved in the programme to visit the laboratory to see it “in action”.
A dedicated courier team collect approximately 12,000 samples per week from 1,200 GP practices and multiple hospital clinics across London.
On receipt at the Halo building, the laboratory team check the samples against request form and book onto the pathology laboratory information management system (LIMS system).
The samples then make their way to the automated platforms for aliquoting and HPV testing.
Negative results are released and authorised within hours. The turnaround time for HPV negative samples is on average five to six days from date of sample collection. On average, 15% of samples will test positive and undergo reflex cytology. As soon as the slides are prepared in the laboratory, they are passed to the screening team.
1,800 samples per week are screened, quality controlled and checked for cytological abnormalities. Approximately 50% will be negative and given a 12-month repeat, 50% will show a cytology abnormality and be sent for consultant reporting.
Behind every well-run operation, there are always countless hidden functions and people responsible for the success of the service.
The consultant team made up of pathologists and consultant biomedical scientists will grade and report abnormal cytology cases. All HPV positive results with cytology abnormality will require further investigation at colposcopy.

Consultants will also prepare and participate in clinical MDT meetings and provide advice to colleagues involved in the management of patients within the programme.
CSL has a proud track record of supporting London Deanery in the training of medical staff. A comprehensive programme has been in place from 2020.
Following the relaxation of covid rules, CSL continues to support sample taker training by hosting visits to the laboratory.
Behind every well-run operation, there are always countless hidden functions and people responsible for the success of the service. Cervical screening has a small team of administration staff who carry out a multitude on a daily basis. These include organising direct referrals to colposcopy units in London who, in turn, will arrange appointments for individuals requiring further investigation. Under the direction of a Failsafe Officer, they manage an extensive failsafe system to ensure no individuals referred to colposcopy are lost to follow up.
The team collate MDT slides and paperwork for consultants to review and handle queries from internal and external agencies.
Another important function performed by CSL is the day-to-day management of the Cervical Sample Taker Database (CSTD) on behalf of NHSE. Sample takers including trainees are assigned a unique PIN number. They must also provide documented evidence to support their training.
Currently, there are 4,000 active sample takers in London.
How has Covid19 affected your work? What steps have you taken to overcome the challenges?
COVID-19 led to massive disruption especially at the beginning of the first lockdown in 2020. Cervical screening in London was suspended except for urgent appointments. All but six of the team were furloughed and did not start returning to work until June 2020 under strict covid-safe measures, including the wearing of masks at all times. Wearing a mask at the microscope did take some getting used to. The company worked hard to keep staff safe by putting screens in place and staff responded by complying with company and government guidance.

The pandemic has helped break down many of the previous barriers that existed and virtual meetings, including clinical MDTs, are now the new and accepted normal. Virtual technology has been key to enabling home working in some specialties such as cellular pathology. Home reporting is not endorsed by the NHS Cervical Screening Programme (NHSCSP), but a project will hopefully be approved later this year to test the feasibility of remote reporting, which will include home reporting of abnormal cervical cytology by consultants.
Increased centralisation will make it difficult for staff to travel the larger distances to the laboratories, so fully tested digital cytology could provide workforce solutions for the future.
The benefits of remote/home reporting can only help recruitment into the profession and retention. The next round of bidding for cervical screening in England may see the numbers of provider laboratories decrease even further; currently, there are eight. Increased centralisation will make it difficult for staff to travel the larger distances to the laboratories, so fully tested digital cytology could provide workforce solutions for the future.
What advice would you give to someone wanting to get more involved in this type of career?
- Visit IBMS website to find out what is involved and the career and qualification pathway for Biomedical Scientists - Home - Institute of Biomedical Science (ibms.org)
- Visit HSL website and explore career opportunities - CAREERS - Health Services Laboratories (hslpathology.com)
- Email the laboratory directly via [email protected] requesting an appointment to discuss career pathways within cervical screening. Where appropriate and safe, we can arrange a visit to the laboratory.
What are the challenges and what are you looking forward to for the future of CSL?
Similar to the wider NHS, the main challenge for CSL is the recruitment and retention of staff. CSL hopes to pilot a remote reporting project in cytology. Enabling remote reporting will increase flexibility and guarantee timely reporting of abnormal cases whilst mitigating against backlogs.
HPV self-sampling is being trialled but not yet available in the NHSCSP. I hope this will become a game changer within the programme and address the issues of coverage.
Digital cytology is not endorsed by NHSCSP but if it is, CSL will be at the head of the queue to embrace any new technology.
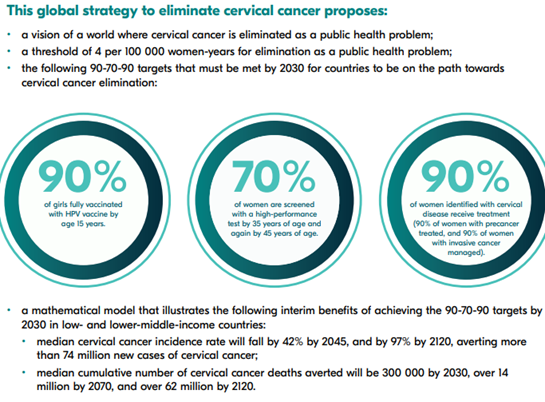
The WHO has set challenging targets across the globe to eliminate cervical cancer by 2030, but the key message for now is to address falling coverage and encourage individuals to attend for regular screening.
HPV self-sampling is being trialled but not yet available in the NHSCSP. I hope this will become a game changer within the programme and address the issues of coverage. HPV self-sampling will greatly reduce the need for clinically taken samples and free up much valued resource within primary care.
What do you think is an important message to share for the cervical screening awareness week this year?
The WHO has set challenging targets across the globe to eliminate cervical cancer by 2030, but the key message for now is to address falling coverage and encourage individuals to attend for regular screening. Even in the age of vaccination, regular screening is key to detecting and treating pre-cancerous changes.