Defining a value proposition
Where should we focus our efforts: reducing cost or increasing the value of laboratory services? Laboratory services underpin modern healthcare at a cost of <5% of the NHS total budget. The value of that spend lies in the effective application of laboratory outputs within processes designed to deliver healthcare benefits to the population served. Those processes are often complex and critically dependent upon laboratory services delivering the right test results, to the right place, at the right time to deliver the right impact. This defines a value proposition (VP) for laboratory services.
From a service provider perspective, the VP describes what is to be delivered by their service model to users; from a service user perspective, the VP describes what is expected from and seen to be delivered by providers. Delivery of the VP therefore requires a common whole system focus from service providers, users and other stakeholders in processes (e.g. clinical pathways) and co-working to define and validate the term ‘right’ within the VP. Once defined, component services within a care system will be able to configure delivery models and outputs that are optimally aligned to deliver desired outcomes with identifiable whole system value. Triple Aim1 provides a framework that can be used to assess the benefits and impact of services across the wider system. However, documentation of benefits in terms of Triple Value,2 which incorporates all the elements of the Triple Aim concept, provides a method of quantifying the whole system value and impacts on total cost of care more suited to the UK healthcare model.
Towards a whole system model
New models of care, emerging technologies, rapid expansion of medical knowledge, and advances in information, data and knowledge management are all drivers for transformation of laboratory services. They also present opportunities to provide higher impact services that result in the delivery of better care. This was recognised in a strategic conference – The end of laboratory medicine as we know it – hosted in Mannheim, Germany, by the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) in 2018. The conference proposed that ‘moving forward, laboratory medicine must redefine its positions, not only acting in its classical role as provider of laboratory results, but also adopting new roles and responsibilities in the clinical dialogue’.3 This requires whole system thinking and involvement by lab professionals with an emerging drive to develop key performance indicators (KPIs) that assess service impact on quality of care and total cost of care. This moves the quality focus on from a traditional introspective focus on lab quality that is of little interest to most service users since it provides no measure of clinical value. Adoption of this new quality construct for laboratory services, with healthcare-targeted KPIs co-owned by service users held jointly accountable for their delivery, will facilitate the necessary whole system and wider stakeholder focus on value. It will promulgate a shared interest in the form and function of laboratory services.
The costs of laboratory tests are a fraction of whole system cost of care (<5%), but they impact significantly upon the overall healthcare spend (the other 95% of the budget). It follows that inclusion of laboratory service providers in healthcare teams tasked with improving quality of care through optimisation of processes within the 95% spend will have a bigger impact on total cost of care.4 This statement is based on the concept of Deming’s chain reaction that identifies the principle that improving processes increases quality and reduces cost of healthcare.5 The important point here is that the suggested primary driver to be addressed is improving processes not costs. It follows that overall healthcare budgets are best managed by managing clinical care, can be improved by elimination of waste and improving clinical outcomes, and can be reduced by eliminating need. Laboratory services committed to the VP identified earlier have an important role in the delivery of impacts in each of these areas. This approach should see laboratory medicine specialists developing in an increasingly important role as change agents in the wider healthcare system, leveraging the benefits of existing and emerging science and technologies.
The recognition and adoption of healthcare-specific KPIs by laboratory services enables their value as clinical services to be objectively assessed and, in turn, provide an evidence base to challenge the historical view that they are costly ‘back office’ services. New KPIs move on from the efficiency-based KPIs to those that, for instance, describe turnaround times to diagnosis, impact on patient flow and capacity, and influence bed stays and drug usage (e.g. antibiotics). The fourth element of the VP – right impact – delivers an explicit requirement for laboratory services to be more outwardly focused and integrated within clinical teams, with new roles and responsibilities within the wider system.
Service transformation in Scotland
NHSScotland’s laboratory programme (NLP, www.labs.scot.nhs.uk) is undertaking work to enable the design and delivery of a distributed laboratory service model (DSM) able to demonstrate efficiency of processes, effectiveness of outputs, equitability of access, resilience and affordability. To enable a service transformation that is value driven, the programme has adopted the VP and a potential improvement model described as the whole system value paradigm (WSVP) to enable delivery. The WSVP identifies four domains that affect the value of a service. Figure 1 provides a representation of the model with high level attributes appended to each of the domains.
Figure 1: The whole system value paradigm
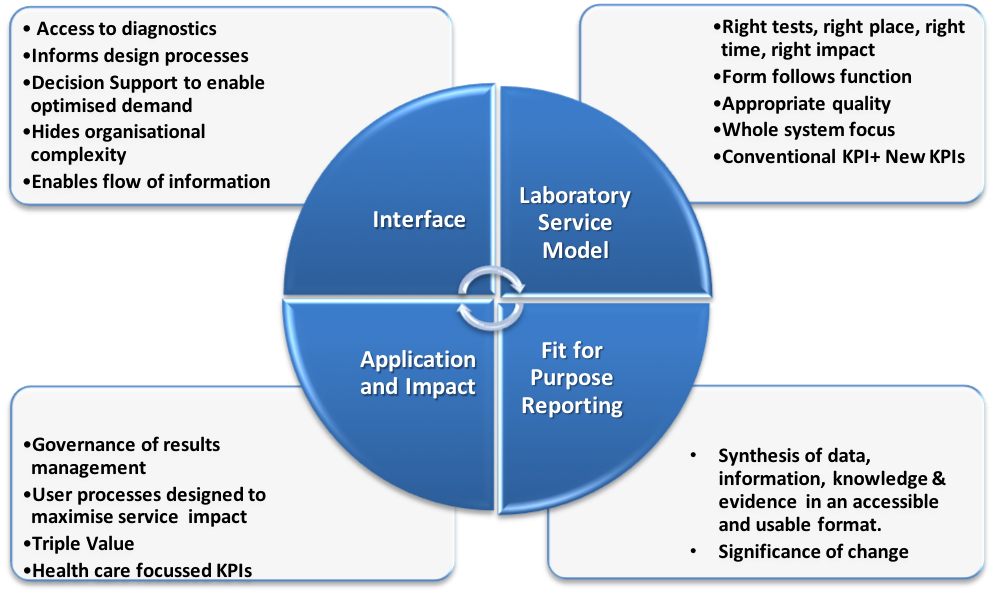
Realisation of the DSM concept demands configuration of services tailored to meet the needs of the healthcare system nationally and at each locality. This requires attention of all service stakeholders to each of the four domains of the WSVP to enable definition of optimal service configurations and delivery of the VP. Clearly the precision of any stakeholders’ focus on each domain will vary, but if they are to collectively achieve their shared aim of delivering desired healthcare outcomes then they must co-produce the final model. This provides the drive to think ‘whole system’ and to explore the wider benefits to justify investment. The model can be applied in a granular fashion, whether at the macro level of a whole service or micro level of a single test, but the focus is always on the same end point of value.
The Triple Value concept is identified as the concept of choice to assess value in the context of the ‘application and impact domain’ of the WSVP. It enables the benefit of services to be identified holistically across the wider healthcare system and categorises impact into:
- allocative value: resources should be allocated to different groups equitably and in a way that maximises value for the whole population
- technical value: quality and safety of healthcare should be improved to increase the value derived from resources allocated to services
- personalised value: decisions should be based on the best current evidence, careful assessment of an individual’s clinical condition and an individual’s values.
The Triple Value concept enables exploration and understanding of the wider impacts of laboratory services within healthcare. The WSVP identifies the domains in which there are processes to be managed/transformed co-productively to deliver better quality of care (Deming’s chain reaction) and thereby address total cost of care. Considering these together, a powerful argument emerges for the transformation of services with value as the primary driver for change and reinforces the view of the EFLM strategic conference that the roles and responsibilities of laboratory professionals must change. If this approach is taken, laboratory services will be viewed as value centres and frontline operations rather than cost centres and back office. The prize is better patient care.
References are available on the College website.

