Oral and maxillofacial pathology (OMFP) is an established cellular pathology subspecialty within the College. There are only a small number of us (36 on the specialist list as at December 2019), yet we disproportionately contribute to head and neck and academic pathology in the UK. The specialty started life as ‘oral pathology’, solely within a dental school environment; the first Chair in Oral Pathology was established in 1944 in Newcastle. The formation of the Oral Pathology Club in 1967, later to become the British Society for Oral Pathology in 1976, laid the foundation for the specialty and in 1967, the first candidate achieved MRCPath in Oral Pathology.1 Further details of the history of the specialty can be found on the British Society for Oral & Maxillofacial Pathology website: www.BSOMP.org.uk. Membership of the Society is not restricted to those from a dental/OMFP background. All who are interested in head and neck pathology are welcome!
While initially the main base of the specialty was dental schools, this has changed appreciably over the past two to three decades. An increasing proportion of the workforce now work in large cancer-focused centres, some of which still retain academic links to a dental school; however, only a minority of the workforce now hold a senior academic position. This change has allowed for expansion of the expertise in the specialty to cover all aspects of head and neck pathology, as will be outlined later. Obviously, there are some areas of overlap with other subspecialties in cellular pathology (most notably ear, nose and throat [ENT] pathology), but OMFP does have a number of truly niche areas, particularly in the lesions involving the teeth and jaws.
OMFP is a dental specialty and is overseen by the General Dental Council (as the appropriate regulator), but with significant input from the College, which, most importantly, oversees the FRCPath in OMFP by examination. Trainees in OMFP must be registered dentists, and most come to the specialty having completed a number of Dental Core Training (DCT) posts and some time in primary dental services. The training is five years (full time) and must incorporate at least one year of general/anatomical pathology rotations (in practice, most trainees do much more than this) (Figure 1). Many incorporate MScs or PhDs into the training pathway, some via the National Institute for Health Research (NIHR)-funded Academic Clinical Fellowship and Academic Clinical Lecturer scheme.
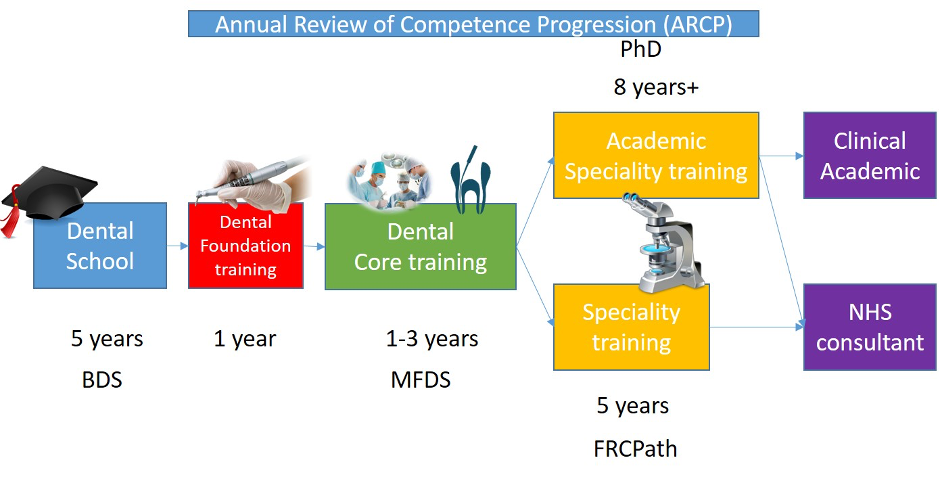
Figure 1: Overview of specialty oral and maxillofacial pathology training from undergraduate to consultant accreditation.
BDS: Bachelor of Dental Surgery; MFDS: Member of the Faculty of Dental Surgery of one of the Royal College of Surgeons.
A day in the life…
In many respects, the daily working life of an OMF pathologist is no different from that of any other cellular pathologist. The main differences lie in the distinction between those who hold academic positions and those who largely work within NHS histopathology services. Those with academic positions will have teaching and research responsibilities in addition to NHS commitments. Many dental schools have retained significant teaching of general, systematic and oral pathology in undergraduate curricula, despite the fashion for dispensing with such, and thus teaching forms a large component of most academic positions.
Other component parts of a cellular pathologist’s life, namely multidisciplinary team meetings, large specimen cut-up (in many centres the small specimens are dealt with by extended practice biomedical scientists) and reporting cases are very familiar. Given the overlap with ENT pathology, many OMF pathologists will routinely report the full range of head and neck cancer resections, including oral cavity, pharynx, larynx, salivary gland and neck dissections, many of which include the bones of the maxillofacial skeleton (Figure 2). This brings a level of anatomical complexity that many find rather daunting, although the judicious use of cut-up photography/radiology helps in this regard.

Macroscopic photograph of mandibulectomy specimen for excision of an ameloblastoma at the posterior aspect of the mandible.
On a wider note, OMF pathologists, both at consultant and trainee level, have been fully engaged with a number of national initiatives that have focused on the reinvigoration of academic cellular pathology, most notably the National Cancer Research Institute (NCRI)-funded CM-Path initiative, where OMF pathologists are involved in every workstream.
Distinctive features of OMFP
The distinctive features of OMFP largely arise from the anatomical complexity of the maxillofacial regions, and the range of tissue types that are present. In this respect, a dental qualification is essential to understand the complex developmental biology of the jaws and teeth, which underpins much of the pathology of the region. Resection specimens from the jaws, particularly if including teeth, strike fear into many experienced pathologists but form part of our everyday work. The combination of background pathology teaching within dental undergraduate curricula and focused training in this particular anatomical subsite results in true specialisation in a number of areas, including:
- odontogenic cysts and tumours that are unique to this region of the body. When combined with the crucial role that radiology plays in their diagnosis, this becomes a very specialist area
- specimens containing bone and tooth tissues, which require decalcification
- teeth specimens that may provide useful features in the diagnosis of a number of developmental conditions
- the diversity of tumours of salivary gland origin, which is much higher than elsewhere in body
- the growing incidence of human papillomavirus (HPV)-related cancers of the head and neck, and the role that HPV may play in dysplastic lesions of the oral cavity
- the effect that exposure to the oral environment, including the oral flora, has on a wide range of lesions of the mucosa of the upper aerodigestive tract, particularly those that are infective in origin, including Candida, tuberculosis, syphilis, HPV and Epstein-Barr virus
- the pathologies related to the branchial arches that result in developmental cystic lesions.
The extent of this expertise in OMFP in a number of the areas outlined above is demonstrated by the very significant contributions of a number of senior OMF pathologists to the 2017 WHO Classification of Head and Neck Tumours, across a wide range of pathologies in the oral and maxillofacial region.2
The future
This is the crystal ball part: cellular pathology is changing rapidly and OMFP will need to change with it. We believe that there are sufficient distinctive features in OMFP to justify its continued existence as both a dental specialty and a subspecialty of the College. In an era with significant workforce challenges in pathology, this is even more crucial. Many of the changes we face are common to all cellular pathologists – the challenges and opportunities of digital pathology, increasing application of molecular tests for diagnosis and therapeutic decisions. These changes are already being applied in salivary gland and mucosal pathology, but will become part of other diagnostic areas, including odontogenic lesions. We need our workforce to have the skills to be able to grasp these opportunities as they come on stream. The other main issue is the continued academic base that underpins much teaching and research in dentistry – will this continue to be supported in dental schools? The future will be challenging, but there is a key role for this small but beautiful specialty to play. Come and join us at the International Association of Oral and Maxillofacial Pathologists congress, which will be held in London in June 2020, if you need to be convinced.


