- Published:
- 17 July 2025
- Author:
- Katy Heaney
- Read time:
- 8 Mins
Point-of-care testing is a growing field of pathology that has advanced rapidly over the last 4 years. It has been recognised by NHS England as an area requiring attention for its potential to improve patient care – when properly implemented. NHS England’s Southeast POCT Group Chair, Katy Heaney, explains more.
In November 2023, the NHS England Pathology point-of-care testing (POCT) subgroup was set up under the National Pathology Stakeholder Board by the pathology transformation team. The group was set up with representation from pathology networks, Getting It Right First Time (GIRFT) and NHS England leads from key collaborative work areas, such as virtual wards and community pharmacy. Volunteers were invited to join breakout workshops on 2 areas: firstly, an audit of POCT, focused beyond the acute trusts, to understand the size of the workload; and secondly, the setup of a community of practice (CoP) to bring together POCT leads.
The audit group initially drafted a questionnaire to gather insights from POCT users within the community, with the aim of creating a baseline for ungoverned POCT. However, progress was hindered by the challenge of identifying respondents who were simultaneously aware of both the specifics of the tests being run and the details of how their service was funded. This information often sits within different roles, raising a risk of incomplete or unbalanced responses.
Complicating matters further, community trust roles are not consistently structured across organisations, making it difficult to identify a single job title or point of contact with the remit to support completion of the questionnaire. This lack of standardisation created barriers to efficient distribution and completion.
Lessons from previous audits conducted by some pathology networks highlighted the inconsistency in responses when attempting broad outreach without clear, local coordination. In response, the original question set was restructured into a suggested audit pack that could be used flexibly by each pathology network, allowing them to gather relevant information on community POCT use once appropriate local contacts had been established.
NHS England’s CoPs have evolved in different ways in the last 5 years. Dependent on one’s involvement, experience with these communities may vary significantly in terms of how they function and the benefits they deliver. In pathology terms, this work would be described as a user group for one of our manufacturers – the coming together of NHS staff working with the same equipment or manufacturer to achieve the same goal, learning from experience and raising shared challenges.
NHS England launched a centrally driven initiative aimed at proving the value of CoPs. While well-intentioned, this push resulted in pressure to establish new communities quickly, sometimes at the expense of allowing them to develop organically in a way that best served the needs of their members. Nevertheless, the POCT CoP is meeting, with a structured membership model of network representation encouraging participants to raise challenges and share best practice.
The best of the discussions from the national group have been on the opportunity to find shared opinions and collaborators on focused topics. For example, this includes identifying which of us are involved in the POCT genetic test trials. We are supporting each other through what is a very new extension to POCT disciplines, laden with very expensive reagents, very limited commercially available quality material, and ethical issues on consent.
Discussions with NHS England pharmacy leads included how the governance of POCT can improve the longevity of investment in a pharmacy POCT installation, building confidence and providing healthcare scientist expertise for troubleshooting problems and challenges. The group has also indulged in a nostalgic conversation on ‘the blue book’ as an example of when national sharing of data on the performance of POCT tests took a more hard-copy approach, but brought enormous benefit to reducing local verification and market understanding of devices. A template is being finalised for proposed sharing of data in a similar way, which we hope will be used to standardise data formatting to make it easy to locate and understand.
The NHS Futures platform brings great opportunity to securely share information and support collaboration within the NHS. If you have not already signed up, I would highly recommend you do so. The National Pathology Transformation Programme workspace includes the POCT section, in which we have begun our key document-sharing initiative. This initiative has sections on business case and service level agreement templates, trust policies, training and competency.
My own vision for POCT is to develop opportunities for collaboration and sharing at multiple levels – international, national, regional and network (Figure 1). International collaboration has improved through International Federation of Clinical Chemistry and Laboratory Medicine initiatives and the use of online webinars to encourage sharing and contact.
The England national group, as described above, continues to evolve; I intend to support it through its transition into the Department of Health and Social Care when NHS England is dissolved. The shift in care from acute to community requires POCT to be well-governed and led by healthcare scientists and pathologists to be effective and cost-efficient. It would be fair to say that Wales and Scotland are ahead of the game, having appointed national leads for POCT; Northern Ireland has had a national group for some time. The role of the regional group for POCT might be new to some but, working with my Southeast regional colleagues, we have shown it to be highly effective and powerful.
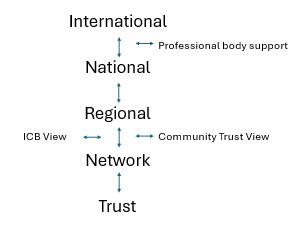
Figure 1. POCT communities – improving the flow of information about POCT to all areas of healthcare is essential to progress.
In April 2024, the Southeast POCT Group was formed with support from our regional NHS England pathology team, with a drive to bring together clinical and operational POCT leads from each network. We allowed flexibility for those networks that were not working as one organisation to send multiple individuals at a trust level as required. We have quickly established a monthly online 1-hour forum for focused discussions and a drive for collecting our data in a uniform way to evidence our work.
Key findings so far
With 21 acute trusts classified as within the Southeast pathology network (South 4 to South 8), we have a significant opportunity to generate large data pools that carry substantial influence. We need to provide evidence for our most staff-poor POCT services to grow. We audited workload and workforce, and compared them to metrics of trust size. The most conclusive correlation was against emergency department admissions and then internally against their UK Accreditation Service (UKAS) status – accredited, applying within 1 year, gap analysis underway, or no active work toward.
We have shared our data locally to support those of us most at risk – single-handed, under-resourced services without assigned clinical leadership, with little connectivity and far off a UKAS application. Sharing this learning helps to support business cases and discussions and, ultimately, has direct implications for patient safety. Failure to improve on these metrics creates risks, such as the possibility of inaccurate results, lower-quality services or the absence of POCT altogether. This can lead to a postcode lottery in healthcare, where patients in one trust benefit from rapid diagnosis, while those in another face delays due to reliance on laboratory testing turnarounds. The audit template has been used in the Southwest to allow regional comparison. We would be pleased to share with other regions to allow them to benchmark themselves too.
Our Southeast region POCT group’s terms of reference, example agendas and minutes are held on the NHS Futures page. Our Southeast diagnostics workspace hosts our Southeast POCT group page, with our minutes and links to reach out to the group. Again, NHS Futures is facilitating a shared space for collaboration of documentation in a secure manner.
I have been encouraging the formation of networks at our national group in those areas that have not formed networks. I see this as particularly important when it comes to assessing community trust POCT provision. Our pathology network boundaries do not neatly meet our community trust boundaries; a regional view of which community trusts are supported for POCT and which are not is useful to establish gaps and begin building relationships. We are nearing completion of our audit of Southeast community trusts, virtual wards and community diagnostic centres to establish any gaps in governance of known POCT services or those that would benefit from them. This mapping exercise comes back to ensuring parity of service provision for our patients in the region.
I encourage all those working in POCT to seek out collaboration at all the levels described above. The POCT community is stronger together and the benefits of collaboration can save time and money. POCT is capable of answering direct questions on patient decision-making and can lead to improvements in specific pathways of care. We must push forward to ensure it is led by pathology expertise and safely used at all stages of a patient’s journey.
Thanks to the National POCT Group leadership, administration and membership, and to the Southeast POCT Group membership and regional pathology team.




