Changes in organ donation legislation
Over the last decade in the UK, there has been a significant increase in organ donation, with the number of donors increasing by 56%. The introduction of opt-out legislation is expected to increase this figure further. The opt-out journey started in 2015 with its introduction in Wales. It was then adopted by Jersey (2019), England (2020) and Scotland (2021), with Northern Ireland, the Isle of Man and Guernsey soon to follow. This tremendous legislative feat was undertaken with the help of multiple individuals and organisations. Overcoming the various logistical, legal and cultural barriers has made the organ donation community even more determined that the new laws should be fully enacted and an individual’s decision to be a donor should be fulfilled.
Statistical impact of the new laws
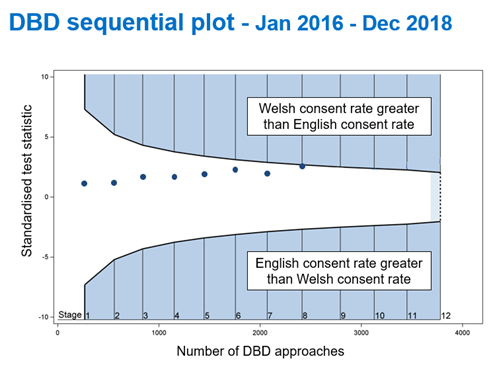
So far, the full impact of the opt-out scheme remains to be seen. Statistical analyses are in progress and the numbers are being closely monitored. The data from Wales was compared with England from the time before donation legislation was introduced. For donors where death has been confirmed by neurological criteria, termed donation after brain death (DBD) donors, a steady upward trend in the proportion of families consenting to donation has been seen. This difference reached statistical significance as seen in Figure 1. Further multivariable analyses have indicated there was an increase in both DBD and donation after circulatory arrest (DCD) consent rates in Wales in the three years following the introduction of opt-out legislation, though the impact seen was not immediate.
Over the last decade in the UK, there has been a significant increase in organ donation, with the number of donors increasing by 56%.
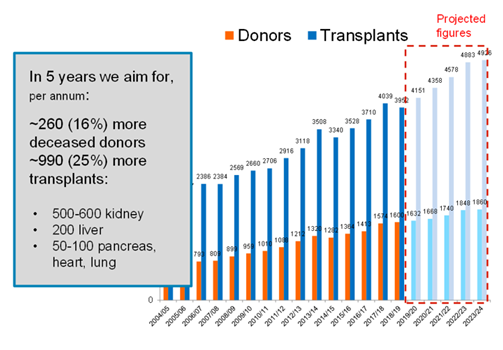
Based on the data from Wales, the statistical experts at NHS Blood and Transplant (NHSBT) have predicted, even with a moderate impact from the legislation, that donation and transplantation will increase with a possible 25% rise in transplants. The UK government was quoted in parliament to expect 700 more transplants per year (Figure 2.)
The impact of COVID on donation
No update in any field of medicine would be complete without a mention of the virus that has, in some way, affected all our lives over the last two years. Organ donation and transplantation across the world have been significantly affected by COVID-19.
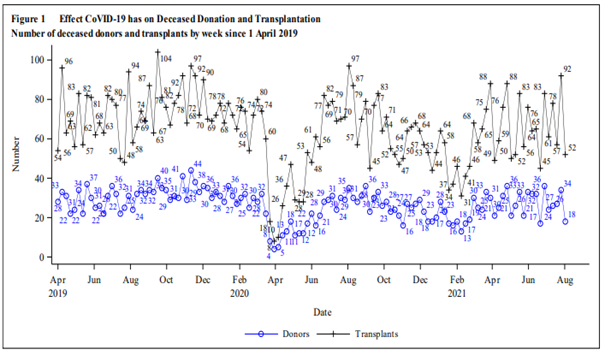
In late 2019, the world was made to pause in many respects and organ donation was no different. Predictably, there was an immediate initial dip in organ donation and transplantation rates in the UK and globally. The potential risks were initially unclear. Hospital surges and demands on intensive care units meant that transplantation services were temporarily halted in all but a few cases. Living donation transplants, with the added worry of the health risk to the donor, were halted. In retrospect, it is amazing that three UK transplant centres managed to remain open during the first wave of the pandemic.
New ways of working
Behind the scenes, however, activity was at a high level and the community was collaborating in a way that was not necessary, or even possible, previously. NHSBT led the drawing together of senior clinical and non-clinical managers, patient group representatives, lay representatives and commissioners from across the UK.
Regular (sometimes daily) meetings addressed problems as they arose, planned for the next wave of the pandemic and immediately enacted decisions that would have taken weeks or months in ‘normal’ times. International collaboration was strengthened with the implementation of weekly calls to enable rapid sharing of experiences. Through this cohesive working, the transplant community recovered and adapted to the changing times with remarkable agility and team working. Clinical teams joined forces and found ways to ensure that the gift of donated organs materialised into subsequent transplants.
Keeping morale high
These were testing times, but the shared purpose of the many donation and transplantation teams kept morale high throughout this period. Tribute must also be paid to the retrieval teams who continued to travel around the country to donor hospitals (where, of course, COVID cases were centred) to carry out the wishes of donors and their families. In the UK, centres worked together in a way that was never seen before, with patients transferring between centres and clinicians working around logistical barriers to ensure transplants still proceeded.
The altruism of donor families in this situation should also be celebrated. Families of donors demonstrated an astounding degree of care and compassion. Despite not being able to visit family members in hospital, record numbers of families consented to organ donation, reflecting the incredible generosity of human nature in times of hardship. Organ donation was brought to the forefront of our minds by unfortunate circumstances, but the way in which it was handled was truly humbling.
Rebuilding capacity
These efforts meant that transplantation rates soon recovered in a manner that was both swift and safe. Information and evidence were collected and collated throughout this period, so by the time the second wave of the pandemic hit, the transplant community was more informed and could respond to the situation with better clarity.
By the summer of 2020, all transplant centres were able to reopen, and deceased donor transplant rates soon recovered to pre-COVID levels (Figure 3). Living donor transplantation has now also recovered and the UK living kidney sharing scheme has resumed, with matching runs being equivalent to pre-pandemic activity in terms of numbers of donors, recipients included and transplants identified.
Transplant safety and COVID
Organ donation guidelines specific to COVID-19 have been developed and are ever-changing as new evidence emerges so donation and transplantation can proceed safely. To date, there is no known transmission of SARS-CoV-2 in the UK through donated organs.
The development of the COVID-19 vaccine has been an extraordinary medical accomplishment globally and the transplant community awaited the developments with interest.
Transplant recipients were classed as vulnerable and were among the first to be vaccinated. Although effective in transplant recipients, the antibody response to the vaccine is less effective than in the general population.
To ascertain the extent of this, analyses have been performed on combined data from the UK Health Security Agency (UKHSA), the National Vaccine Registry and NHSBT Registry. Unvaccinated patients were found to be at significantly higher risk of severe disease if they contract SARSCoV-2 infection in comparison with vaccinated patients.
A rare complication following immunisation with the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2 is vaccine-induced thrombosis and thrombocytopenia (VITT). The consequences of proceeding with transplantation from donors deceased from VITT were closely monitored and UK guidance has been drawn up for the selection, recovery and transplantation of organs from donors with VITT, as well as recipient monitoring.
The importance of multidisciplinary working
Our colleagues in the histocompatibility specialty have also had to rapidly adapt and have been involved in vaccine efficacy trials. Reports of allosensitisation have been reported after vaccination, as has been the case with previous vaccines. There has been an enormous research effort in this area. Indeed, these colleagues have once again demonstrated that their expertise is essential to support timely decision-making in transplantation and the vital role that this service plays in organ donation and transplantation must be highlighted.
Those in histopathology who give opinions on biopsies of donor organs or abnormalities at the time of donation are increasingly important to the service when considering donors with increasing age, comorbidities, past history of carcinoma and potential infectious disease transmission. This information is often critical to proceeding with transplantation.
Changing attitudes to organ donation
As well as scientific progress during the pandemic, cultural advancements have also been made and many communities from different backgrounds have been brought together. For example, the introduction of opt-out legislation led to greater engagement with faith communities, with collaboration to improve community engagement and education regarding the organ donation process and address common misconceptions about the process. As part of the commitment to provide support for organ donation amongst communities, NHSBT has developed the Community Investment Scheme, which provides funding for trusted organisations to help drive awareness within communities.
NHSBT has also worked with faith leaders and communities to build trust, raise awareness and discuss the barriers to organ and/or tissue donation and how organ donation can proceed in line with faith or beliefs. As a result, as part of joining the organ donation register, a statement is now included which can be ticked regarding whether NHS staff should speak to family members about how organ donation can go ahead in line with an individual’s faith or beliefs.
Improving transplant services
To help ensure that as many lives are saved as possible through the introduction of opt-out legislation, there is a new focus on improving transplantation services and organ utilisation. The Secretary of State for Health and Social Care has established a new Organ Utilisation Group to make recommendations on how to improve the transplantation system and reduce current geographic and ethnic inequities in access to transplant services. It is anticipated that this will lead to a revolution in transplantation services, in the same way as the Organ Donation Taskforce recommendations did for deceased organ donation services.
In addition, Clinical Leads for Utilisation have been established in all UK transplant units to identify and address local barriers to organ utilisation. There is also work underway to bring the organ donation and transplantation teams closer together and work collaboratively to ensure that there are no missed opportunities for successful donation and transplantation.
The field of transplantation is a demanding one to work in ... but the rewards are immense in seeing the transformational power of the transplant procedure.
The future of transplantation
There is still a long road ahead in the future. Thousands of patients await life-saving and life-improving transplants, and much work is yet to be done to help reduce this number. The Organ Utilisation Group is providing focus and motivation to teams to deliver improvements – but we need to make sure this impetus is maintained.
The field of transplantation is a demanding one to work in. Unsociable and long hours make for a relentless work schedule, but the rewards are immense in seeing the transformational power of the transplant procedure. The workforce is dedicated and motivated. The next challenge is to maintain the enthusiasm, help prevent the widespread burnout that is affecting NHS workers as a whole and to entice young colleagues to join the organ donation and transplant community, and indeed to remain a part of it.
The UK drives innovation in transplantation and is a world leader in many aspects of the field including DCD donor transplantation. We are at the forefront of much of the novel research being conducted, for example, in machine perfusion techniques. On the horizon, the challenges that await us include ensuring that UK organ donation maintains the excellent standards that are currently being held and continues to deliver world-class healthcare.






