What is an amber alert?
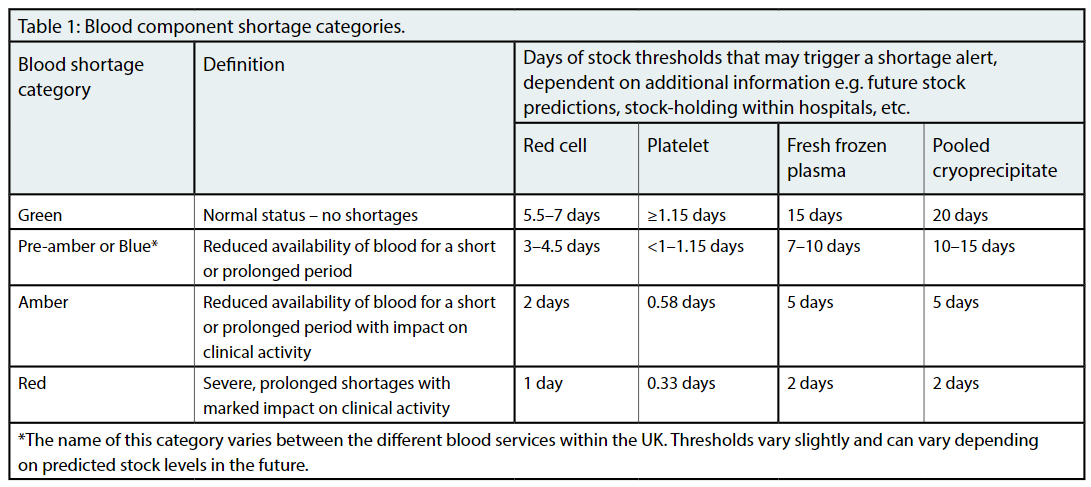
NHS Blood and Transplant (NHSBT) usually aims to hold around six days' supply of red cell compo-nents to maintain the blood supply within England. An amber alert occurs when there is a significant risk to the supply of blood that will affect clinical care. An amber alert for red cells is usually trig-gered when blood stock levels in a particular group fall to below two days’ supply (Table 1).1 In October 2022, there were shortages of red blood cells across multiple blood groups and stock levels were predicted to become even lower unless action was taken to decrease red cell usage. Reducing blood use helps to maintain the blood supply for all urgent and life-saving transfusions.
The National Blood Transfusion Committee (NBTC) has produced guidance on what to do during a shortage situation, suggesting measures that should always be in place, such as patient blood management.1–3
Why did it happen?
It occurred for multiple reasons. Maintaining blood stocks has been an ongoing challenge in the after-math of the COVID-19 pandemic and stock levels were low over the summer. There was, therefore, little resilience within the system when any further reductions in blood collection occurred. This reduction in stock levels occurred across all blood groups.
NHSBT is experiencing ongoing staff shortages, caused by increased staff turnover and the impact of recruiting and training new colleagues. This left NHSBT vulnerable to short-term sickness and, in common with the wider NHS and other services, there were high levels of COVID-19 absence during September and October 2022. This led to appointments to collect blood from donors being cancelled.
Higher staff turnover meant that there was a higher proportion of new staff in training and, therefore, fewer staff able to collect blood dona-tions. It also meant that there was a higher proportion of newly trained staff. It takes time and practice to become an expert at collecting blood donations. This led to fewer donations collected per trained member of staff.There have also been recent changes in donor behaviour. Footfall fell around many city centre donor centres, such as Leeds and Manchester, as many donors were working from home. The foot-fall in some large donor centres, such as the West End Donor Centre near Oxford Circus, has still not recovered to pre-pandemic levels, leading to fewer donations occurring.
What was NHSBT’s response?
NHSBT has changed multiple processes in the recruitment and retention of donor carers (the main staff group who collect blood donations). NHSBT has developed new training approaches, including a training academy and training sessions alongside a normal donation session. It has nearly doubled the staff who provide training in blood donation to increase the level of support and development of trainees. This has already led to a decrease in staff turnover. There has been an active recruitment campaign to increase the number of staff members, which is continuing into 2023. There have been multiple donor campaigns with local and national media to increase blood donation, as well as direct contact with individual donors. This has led to an increase in the number of donors booking an appointment to give a blood donation, as well as increasing the number of available appointment slots.
NHSBT also asked other UK Blood Services for help. The UK Blood Services support each other if one has a shortage of blood components. However, NHSBT collects approximately 84% of all blood components donated within the UK, so a blood shortage within England cannot be mitigated by support from the other UK Blood Services.
NHSBT communicated with all hospitals, including chief executives and medical directors, as well as the Department of Health and Social Care and NHS England’s (NHSE) Emergency Preparedness, Resilience and Response team. It liaised with all medical royal colleges, the National Blood Transfusion Committee, National Transfu-sion Laboratory Managers’ Working Group, British Society for Haematology, British Blood Transfusion Society and other relevant societies. Many of the royal colleges and societies communicated with their members to highlight the blood shortage situ-ation and what could be done to mitigate the issues it caused.
The Blood Stocks Management Scheme created individualised red cell stock-holding guidance based on the data each hospital had submitted over the previous 12 months on stock-holding and wastage. This highlighted how red cell stock could be reduced to minimise wastage within each hospital.
The National Comparative Audit provided personalised summary reports to all hospitals, highlighting how hospitals performed against the NICE blood transfusion quality standard during the 2021 NICE Blood Transfusion [QS138] Audit.4,5 This data was also uploaded to the Model Health System so that hospitals could compare their performance against other similar hospitals.6
What did NHSBT ask hospitals to do?
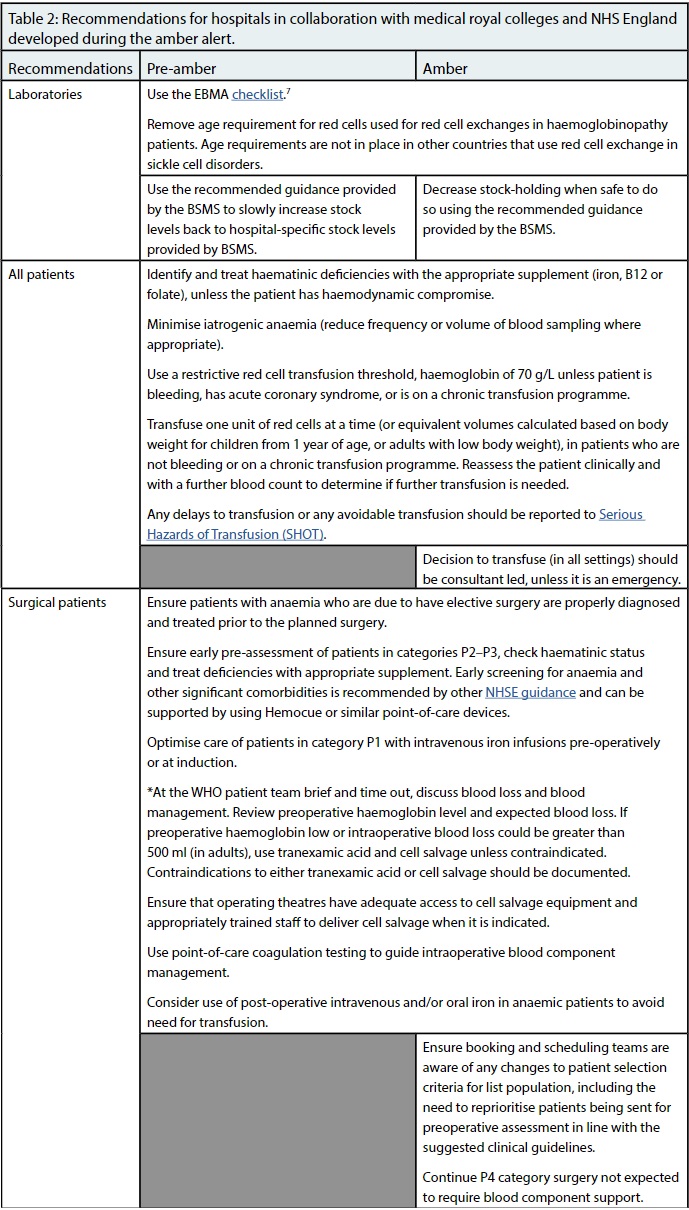
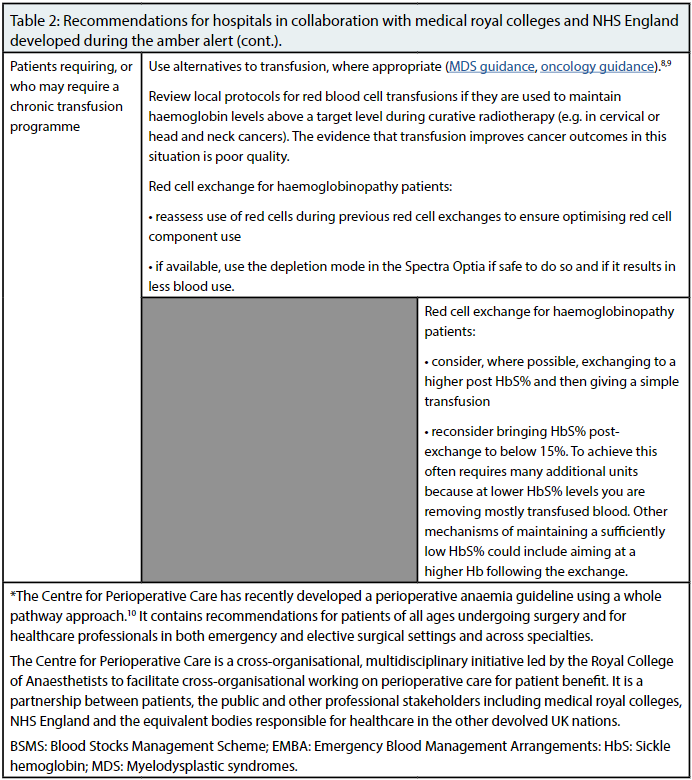
NHSBT asked hospitals to follow their Emergency Blood Management Arrangements (EBMA), using the NBTC checklist as a guide.7 It also worked with hospitals, medical royal colleges, NHSE and other relevant bodies to develop guidance (Table 2). This guidance mainly comprised good practice based on national and international guidance, including the NICE guide-lines for blood transfusion and other patient blood management good practice guidelines.8–11 Surgery that could be delayed for more than three months and was likely to require red blood cell component support was recommended to be postponed (reduced to Priority Level 4).12 Nearly all surgery within this category did not require blood component support and could continue without any limitations.

What did we learn from the amber alert?
Hospitals, with support from the relevant medical royal colleges and professional societies, were all very helpful and responded to the appropriate guidance to decrease blood usage. Blood donors responded to the call to donate, which led to 100% of appointments being filled in the time during the amber alert. NHSBT could not have improved the blood stock situation without everyone’s help.The overall impact of all the measures used was to decrease blood usage by around 20%. Together with increased blood collection, this led to the amber alert ending on 8 November 2022, moving into pre-amber status. As of 1 December 2022, NHSBT remains in pre-amber.
The decrease in demand for red cell components was due to a combination of factors. Firstly, it was caused by a significant decrease in stock-holding within hospitals from an average of 5.5 days of red cell stock held within hospitals to around 3.5 days of stock held. The second cause was a significant increase in the use of alternatives to red cell trans-fusion, including increased use of tranexamic acid prior to major surgery, use of iron therapy when indicated and use of red cell salvage techniques during surgery. Thirdly, demand fell due to the use of more restrictive transfusion thresholds for all patients. The postponement of some surgery was likely to have been of limited benefit due to the small number of patients affected.
NHSBT and the NBTC will continue to learn lessons from this amber alert and, in conjunction with others, will use this knowledge to revise blood shortage plans for the future, as well as continuing to build resilience in the blood supply chain.
Acknowledgements
Everyone who helped to support blood supply by increasing red blood cell collection and decreasing red blood cell usage.