Novel treatments for haemophilia are exploiting advanced genetic therapies, with many promising results reported and beneficial treatments in development. Current trials are working with the genetic code to transform the outlook for patients with haemophilia.
Haemophilia A and B are rare, X-linked inherited conditions caused by either a lack or a deficiency in clotting factor VIII (FVIII) or factor IX (FIX), respectively.1,2 Haemophilia A has an estimated prevalence of 1 in 5,000 live male births. Haemophilia B is much rarer, with a prevalence of 1 in 30,000 live births.3,4 Although these bleeding disorders were first referenced in the 2nd century AD,5,6 it is only over the last 70 years that treatment of the conditions has advanced. This is a result of a greater appreciation of the underlying pathophysiology and genetic abnormality.
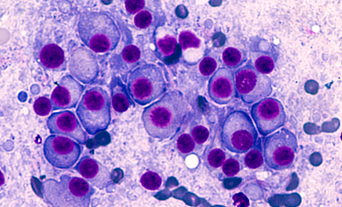
Pathophysiology of haemophilia
Haemophilia A was first described as a deficiency of clotting FVIII in 1952.1 Alongside FIX (which is deficient in haemophilia B), FVIII is key to the amplification and propagation of thrombin production during haemostasis.7 In healthy individuals, FVIII and FIX are activated to form a complex that, in turn, activates FX. Deficiency of one of these factors results in decreased thrombin production and diminishes the ability to produce a stable fibrin clot.
Clinically, the conditions are characterised by bleeding, predominately into larger joints. Progressive bleeds subsequently result in painful arthropathy that limits mobility. Life-threatening bleeding, such as intracranial or internal organ bleeding, is associated with severe cases, but can occur at any level of severity.
The classifications of the severity of both haemophilia A and B are based upon the residual levels of either FVIII or FIX, which in turn are determined by the class of causative variant.9,10 Severity is defined as follows: severe (<1 international unit [IU]/dl), moderate (1–5 IU/dl) or mild (6–<40 IU/dl). The level of factor activity alongside clinical symptoms is used to guide treatment.
Gene therapy represents a natural progression in treatment ... now, the future aim is to provide the patient with the genetic code to produce endogenous factor...
Early treatment methods
Mortality and morbidity due to complications of haemophilia were initially transformed using plasma-derived factor concentrate by pooling donations.11 This development meant that concentrated factor could be given prophylactically at home, preventing bleeding and further joint damage. Tragically, this led to transmission of HIV and viral hepatitis through the use of untreated virally contaminated product. It was estimated that half of British haemophilia A patients contracted HIV, with a reported 1,246 cases.12,13
The infected blood scandal added impetus to the development of a pure donation-independent factor product. The identification and isolation of factor VIII protein and the discovery of the corresponding genetic code in 1984 were critical in enabling recent advances in haemophilia A treatment.14

Although the development of recombinant factor replacement therapies has enabled safe treatment to be given to haemophilia patients, it is still cumbersome and represents a significant treatment burden to patients. Even with extended half-life products, intravenous treatment is required every 3 to 4 days in haemophilia A and every 5 to 15 days in haemophilia B. This leads to peaks and troughs of factor levels, meaning that patients with haemophilia need to plan periods of intense physical activity around their infusions.
Developments in haemophilia treatments
Non-factor replacement therapies
Over the last few years, non-factor replacement therapies have also been introduced to the treatment landscape. The main one is emicizumab, a bispecific FVIII mimetic antibody for haemophilia A. Emicizumab contains 2 different antigen binding fragments and can recognise both FIX/FIXa and FX/FXa. Therefore, it can facilitate FIXa-mediated FX activation by bringing both FIXa and FX into proximity.15,16
The unique mechanism of action of emicizumab provides patient benefit irrespective of the presence or absence of an inhibitor to FVIII. It also places a lower treatment burden on the patient, with a less intensive treatment regimen and the benefit of subcutaneous administration.17 Other subcutaneous rebalancing agents, such as anti-tissue factor pathway inhibitors (TFPIs), are currently being investigated in haemophilia.18 This novel class acts by binding to the Kunitz-2 domain of the TFPI, thus preventing binding of the TFPI to FXa and subsequent inhibition of FXa.19
Gene therapy
Gene therapy represents a natural progression in treatment. Previously, the goal was to develop a donation-independent product; now, the future aim is to provide the patient with the genetic code to produce endogenous factor, thus ameliorating the condition and reducing treatment burden. As a single-gene disorder, haemophilia is an ideal candidate for gene therapy. Those with severe haemophilia are likely to benefit most, as even slight improvement in expression level would have a transformative effect on morbidity and mortality.
This treatment technique relies on viral vectors to transduce therapeutic genes into a target somatic cell. Viruses are highly adapted to transduction, as they transfer their own genetic material during their life cycle. Engineered adeno-associated virus (AAV) was selected as a candidate vector over lentiviruses and retroviruses, as AAV is a non-pathogenic virus with relatively low suitable viral vector for gene therapy studies.20
Specific subtypes of AAV show a remarkable tropism for the liver, making AAV an ideal candidate for use in clotting factor disorders. Initial progress was made with haemophilia B, owing to challenges related to the size of the FVIII gene in haemophilia A. The gene coding FVIII is 7 kilobases (kb) in size, while an AAV can only accommodate 4.7 kb before compensating its efficacy. The realisation that the B-domain of the FVIII gene was not critical to the coagulation process enabled its removal to create a much smaller gene of 4.3 kb that could fit within the vector capsid.21

Clinical advances in gene therapies
From trials to approval
Recent advances in promising clinical trials are close to making this dream a reality. Initial studies on haemophilia A have demonstrated clinically significant results for patients and a transformation in their care. Maintained expression of the gene product has been reported in a phase 3 study at 3 years, with mean levels of FVIII of 18.8 IU/dl and subsequent reduction in bleed rates by 80% and factor concentrate use by 94% compared with baseline.22 Progress in gene therapy has advanced to the degree that valoctocogene roxaparvovec has been granted conditional marketing authorisation by the European Commission (EC).23 A haemophilia B gene therapy, etranacogene dezaparvovec, displayed a durable factor expression at 18 months (34.3%, 95% CI range: 29.5–39.1), with no serious treatment-related adverse events and has recently been granted FDA approval and EC conditional marketing approval.24
For the first time since the condition was first described almost two millennia ago, we are on the cusp of being able to revolutionise haemophilia treatment.
Factors affecting efficacy
While gene therapy offers the chance of a once and-for-all treatment for haemophilia, it is not without challenges and is unlikely to be suitable in all cases.25 Gene therapies have, so far, revealed a high degree of variability in attainment and level of factor expression between patients.26 The underlying cause of this variability in response is not currently fully understood. Suggested factors affecting response include genetic differences, medical history and pre-existing liver disease.25,27 Pre-existing immunity to AAV is common, as it is a naturally occurring virus. There is a concern that anti-AAV antibodies may be able to neutralise the infused AAV vectors. A study of UK haemophilia centres reported anti-AAV5 and anti-AAV8 antibodies in 21% and 23% of patients, which had a neutralising effect in 25% and 38% of cases. Targeted selection of patients without pre-existing immunity is likely to be necessary to ensure maximal benefit from gene therapy.28 However, the HOPE-B trial in haemophilia B did not target patient selection for AAV antibody status and yet has reported a stable and durable factor response.29
Causes for concern
Gene therapy is unlikely to be without side effects and concerns have been raised about the risk of thrombotic events secondary to supraphysiologic factor activity levels. Indeed, an arteriovenous fistula thrombosis occurred in a haemophilia B patient following treatment with verbrinacogene setparvovec; in this case, FIX levels increased to supraphysiological levels of 279 for a sustained period.30
Another side effect, transient hepatocyte cytotoxicity, is common, with 85.8% and 35.1% of participants in the valoctocogene roxaparvovec phase 3 gene therapy trial demonstrating transient elevation in alanine aminotransferase and aspartate aminotransferase, respectively.31 The precise cause of this liver toxicity has not been identified, due to difficulty replicating it in animal models. This transient liver function derangement was treated with corticosteroids. Studies to assess longer-term effects on liver function are ongoing.
In the longer term, there is a theoretical risk of insertional oncogenesis through integration of transgenic material. Although AAV is a non-integrative virus, low-level integration has been noted to occur at between 0.1 and 1% of transduction events.32 Vexatiously, this risk is not likely to be fully realised until trial participants are well outside the initial trial observational periods.25
A case of hepatocellular carcinoma has previously been identified in a gene therapy patient enrolled on the HOPE-B trial. In this case, genomic sequencing suggested that the cancer was related to pre-existing risk factors, including a history of hepatitis B and C, rather than gene therapy.33,34 Cases of salivary gland carcinoma and B-cell acute lymphoblastic leukaemia within the valoctocogene roxaparvovec trial were similarly found to be unrelated to gene therapy. The details of these cases are awaiting publication.35,36
An exciting prospect
For the first time since the condition was first described almost two millennia ago, we are on the cusp of being able to revolutionise haemophilia treatment. The published evidence from the gene therapy trials in haemophilia encouragingly report maintained factor expression and vastly diminished bleed rates. While this is an exciting prospect, it is unlikely to benefit all patients and we need to continually innovate and expand the treatment landscape.