Multiple myeloma has a poorly understood genetic origin and understanding genetic heterogeneity is critical in developing better targeted treatments against the disease. This article reviews the disease and the major barriers to its treatment.
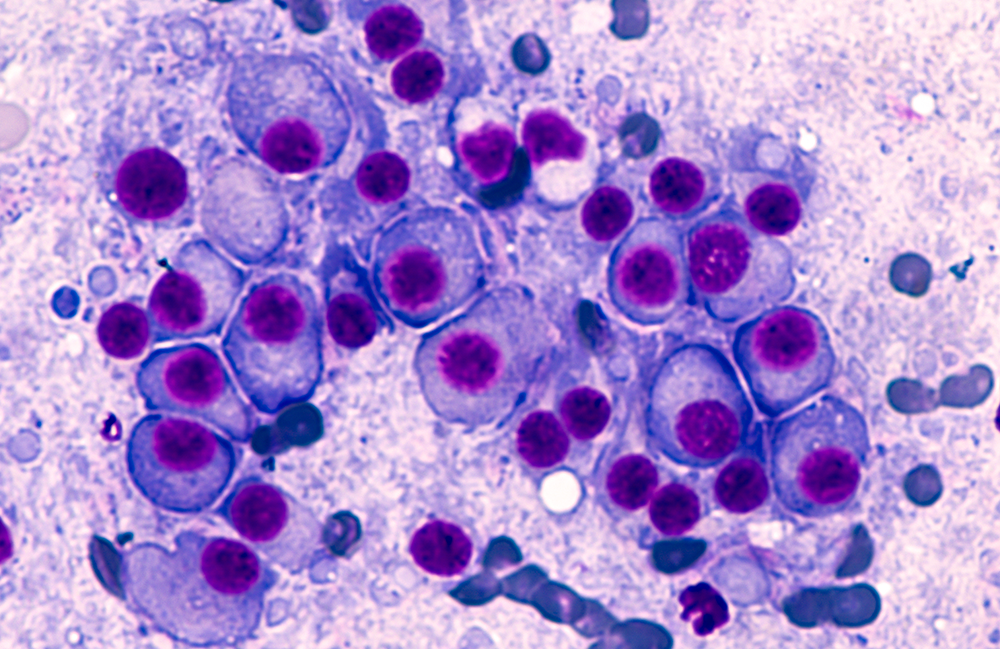
Multiple myeloma (MM) is a malignant disease of plasma cells in the bone marrow. It is characterised by the production of a monoclonal immunoglobulin molecule and serum free light chain and is associated with patchy bone destruction, anaemia, infection and renal failure. MM always arises from a background of an incidental benign precursor condition, termed monoclonal gammopathy of uncertain significance (MGUS), which usually goes undetected in life. Myeloma follows a remitting and relapsing course, with most patients responding to initial therapies but eventually developing resistant disease.
One of the major advances in genetics is the recognition that 25% of patients with poor prognostic genetic markers need to be treated differently. This is leading to the start of an era of more targeted therapies.
Understanding the pathogenesis and biology
MM arises from a background of MGUS and is complicated by poorly understood genetic heterogeneity. Some cases are initiated by primary translocations involving the immunoglobulin heavy chain locus on chromosome 14q32 and a promiscuous range of partner chromosomes.
Although complex, heterogeneous and mechanistically different, genetic events ultimately target key biological pathways, namely DNA damage repair, MAPK, NF-kB, myc, cell cycle, adhesion and motility, and cell differentiation, to name a few. Multiple heterogeneous myeloma sub-clones likely exist in each patient; clonal evolution is a key feature of transformation. Eventually, end-stage myeloma is characterised by the dominance of a treatment-resistant myeloma that frequently becomes independent of the marrow micro-environment.
One of the major advances in genetics is the recognition that 25% of patients with poor prognostic genetic markers need to be treated differently. This is leading to the start of an era of more targeted therapies.
There is a close relationship between myeloma cells and the marrow micro-environment, which promotes tumour growth, chemoresistance and myeloma bone disease. Increased osteoclast activity and corresponding reduced osteoblast activity lead to lytic bone disease. Immune dysfunction leading to infection is a major cause of morbidity and mortality. Renal impairment is common (due to light chain cast nephropathy, most commonly) with 10% of patients on dialysis; it is potentially reversible, if treated early.
Diagnosing myeloma
The problem of delayed diagnosis
Delay in diagnosis is common, owing to the non-specific symptoms (pain, infection, fatigue) and the relative rarity of the condition. In the UK, over 50% of patients have 3 or more primary care consultations prior to a diagnosis, over 20% present via a secondary care pathway and about a third of patients are inpatients at diagnosis. There is a significant early death rate of around 10% and a significant morbidity from delayed diagnosis.
Although education of healthcare professionals is clearly important, the problem of late diagnosis can only be tackled through artificial intelligence in laboratories to alert healthcare professionals of the need to test for myeloma. Screening would also help avoid the problem of late diagnosis. However, in the absence of any early intervention in asymptomatic MGUS patients, an inability to identify those most likely to progress and the crippling costs of monitoring MGUS patients (guessed to be around 500,000–1 million people in the UK), it is unlikely to be supported.
The problem of late diagnosis can only be tackled through artificial intelligence in laboratories to alert healthcare professionals of the need to test for myeloma.
The challenge of access to cross-sectional imaging
Pain arising from the skeletal complications of myeloma is the most common presenting symptom. International and UK guidelines, including those produced by the National Institute for Health and Care Excellence (NICE), recommend cross-sectional imaging (PET-CT and MRI are preferable to plain CT) for patients with suspected myeloma. However, cost and capacity are continuing major barriers to access these.
Plain X-rays are much less sensitive at detecting and characterising bone disease than cross-sectional imaging techniques, which can also show extramedullary disease. Functional imaging, namely PET-CT and diffusion-weighted MRI, are useful for monitoring. At relapse, there is an increasing tendency to form extramedullary tumour deposits that must be detected and monitored with cross-sectional imaging.
When to investigate and when to start treatment
There is no universally agreed definition of what constitutes a patient with suspected myeloma, owing to its heterogeneity. A diagnosis should include any patient with a monoclonal protein and potential signs of myeloma, or a well patient with a monoclonal protein IgG >15 g/L, IgA >10 g/L or clonal serum FLC >500 mg/L.
The urgency with which both a bone marrow biopsy and cross-sectional imaging should be carried out depends on the extent of organ damage. A common and difficult clinical decision is when to start treatment in patients with incidental smouldering myeloma, which is found increasingly commonly.
Can minimal residual disease change treatment?
Improvements in treatments have led to an increasing number of patients having a marrow that is negative for minimal residual disease (MRD), with less than 1 myeloma cell in 105 nucleated cells after induction treatment. MRD response is a powerful prognostic post-induction (but not after relapse). It is likely to have increasing use as a primary endpoint in trials as a surrogate marker of progression-free survival and overall survival. The assessment of MRD is currently performed by either next-generation flow cytometry or next-generation sequencing of bone marrow. Achieving MRD negativity is less common after treatment of relapsed disease and disparities between imaging and marrow MRD assessment are increasingly seen. Future trials will explore using response criteria, namely MRD responses, to direct treatment decisions. But, as yet, there is no objective evidence to use MRD response to alter treatment and there is a worrying trend for clinicians to over-interpret MRD results.
Lack of research into the general aspects of care
Supportive care plays an increasingly important role in the modern management of MM. Modern treatment has significantly improved the outcome for patients with myeloma through improved disease control. However, the vast majority of patients live at home with the burden of the disease itself and the cumulative side effects of treatments. These areas are very poorly researched and include acute and chronic kidney injury, neuropathy due to treatment, bone disease, spinal disease, pain control, anaemia, cardiovascular risk factors and infection.
Assessment of frailty and fitness for treatment has always been done subjectively, but there is increasing interest in objective scoring systems of fitness to direct dosing of drugs. Prophylactic antibiotics are beneficial, as is vaccination, although less effective than in healthy individuals. Certain patients with recurrent infections may benefit from immunoglobulin replacement, but there is lack of data and immunoglobulin is currently a limited and expensive resource.
The treatment of myeloma
Promising treatments
The choice of initial therapy is determined by a patient’s age, frailty, comorbidities, performance status, renal function and access to high-cost drugs. Induction regimens generally involve a combination regimen with up to three novel agents with a steroid. Autologous stem cell transplantation remains a standard approach in fitter patients, typically those younger than 70 years old.
In the year 2000, treatment was mainly limited to alkylating chemotherapy drugs (melphalan, cyclophosphamide), steroids and autologous stem cell transplantation. The explosion of newer treatments started with the use of immunomodulatory drugs (thalidomide, lenalidomide, pomalidomide) and proteasome inhibitors (bortezomib, carfilzomib, ixazomib), and then monoclonal antibodies targeting CD38 (daratumumab, isatuximab).
End-stage patients are commonly a frail, comorbid and treatment refractory population. This is challenging for clinical trials. There are many promising novel agents in MM, which is obviously great news but makes sequencing of combination therapies increasingly complex.
These treatment advances mean myeloma is now a chronic disease for a significant proportion of patients able to live at home...
Monoclonal antibodies
The anti-CD38 antibody, daratumumab, is now incorporated into induction regimens, given its great efficacy, unique mechanism of action and tolerability as a subcutaneous injection. Isatuximab is an alternative anti-CD38 monoclonal antibody.
Promising new agents are the antibodies directed against B-cell maturation antigen (BCMA), referred to as anti-BCMA antibodies. Belantamab mafodotin was the first BCMA antibody and was followed by the more effective BITE antibodies (teclistamab and elranatamab) that bind to both BCMA on myeloma plasma cells and CD3 on T cells. Remarkable response rates of 60% are seen with these BITE antibodies in patients refractory to all previous treatments. Another target is GPRC5D that is targeted by the antibody talquetamab.
Cellular immunotherapy: CAR-T cells
CAR-T cell studies also use BCMA as a target. This involves collecting patient T cells and manipulating them ex vivo to express a chimeric B–T-cell receptor. This is followed by lymphodepletion and reinfusion of the manipulated CAR-T cells, with impressive response rates, although relapse is still common.
There are different outcomes between the various CAR-T cell studies and longer follow-ups are needed for all these studies. Cilta-cel (Janssen) and Ide-cel (BMS) are the most advanced CAR-T cells used in myeloma; both have been licensed by the FDA and both have shown excellent efficacy in heavily treated patients in the KarMMa (Ide-cel) and CARTITUDE trials (cilta-cel).
Toxicity is also an issue, with cytokine release syndrome, neurological toxicity and profound immunosuppression with high infection rates. But the main issue will be cost and the very limited capacity to make and deliver CAR-T cells. Other CAR-T cells are in development against BCMA and also other targets.
Targeted therapies
Treatments that are developed for specific genetic subtypes of myeloma are still in their infancy. Examples of truly targeted therapies include the drug venetoclax, which works specifically in the 15% of patients with myeloma who have the t(11;14) translocation. This translocation leads to higher expression of anti-apoptotic protein Bcl-2, which is the target for venetoclax. BRAF inhibitors can target the 4% of patients with a BRAF mutation. Signalling inhibitors trials are ongoing but have yet to deliver into clinical practice.
A chronic disease, financially challenging and still incurable
Myeloma is now one of the most expensive cancers to treat. Patients must have multiple lines of expensive agents in combination. There is a large difference between what is licensed and what is affordable for most healthcare systems (NICE and Cancer Drugs Fund in the UK). It accounts for less than 2% of cancers but consumes up to 15% of the cancer drugs’ budget.
These treatment advances mean myeloma is now a chronic disease for a significant proportion of patients able to live at home, but the ability to deliver repeated treatments is a limiting factor for the majority of older, frailer patients. Despite these advances, treatment is typically continuous and eventually myeloma develops into a refractory disease with a poor outcome.




