Staying true to the core role of pathologists, and the College’s motto, the theme for the April Bulletin is ‘The science behind the cure’. Here, Bulletin Editor Dr Shubha Allard introduces the articles that celebrate the scientific advances behind the diagnosis, treatment and prevention of disease.
According to legend, the Holy Grail was the cup used by Jesus at the Last Supper and has been the quest of many a knight. One could argue that the so-called quest for the Holy Grail continues in modern medicine, where the term is used to describe the search for a highly difficult outcome that feels almost mythical. Our theme for this April Bulletin, ‘The science behind the cure’, certainly encapsulates the various fields in pathology where such a quest seems to have had welcome results.
...gene therapy for haemophilia represents a natural progression in treatment...
Pathogenesis of haemophilia
Alan Mitchell and Priyanka Raheja eloquently cover the journey from the first description in the 1950s to the better understanding of the pathogenesis of haemophilia A and B and a full elucidation of the genetic basis of these two disorders. The advent of treatment by replacing the deficient factor with plasma-based concentrates completely modified the significant morbidity and mortality related to serious bleeding. However, there were many pitfalls related to transfusion-transmitted infection, including HIV and viral hepatitis; these issues are still being scrutinised as part of the current infected blood enquiry.
Purer factor concentrates and, indeed, recombinant technology have resulted in improved replacement therapy, but this is still onerous for patients. Non-replacement treatment, in particular emicizumab, a bispecific FVIII mimetic antibody, represents a further advance as a less intensive treatment regime.
As haemophilia is a single gene disorder, gene therapy represents a natural progression in treatment, but this has felt like a quest for the Holy Grail for at least two decades. This treatment technique relies on viral vectors to transduce therapeutic genes into a target somatic cell. Initial progress was made with haemophilia B, with the size of the FVIII gene in haemophilia A posing challenges. Removing the B-domain of the FVIII gene, as it is not critical to the coagulation process, leaves a much smaller gene of 4.3 kb that readily fits within the vector capsid.
Considerable progress has now been made, with conditional marketing authorisation by the European Commission for gene therapy options for haemophilia A and B. While trials report maintained coagulation factor levels and vastly diminished bleeding, gene therapy will not be the panacea for all patients and does also have side effects, so the need for ongoing innovation continues.
Genome editing may support the production of non-immunogenic ‘universal’ blood cells...
In vitro red blood cells
Growing an unlimited supply of red cells in vitro for clinical transfusion, fulfilling the bespoke needs of patients and obviating the need for donor blood, certainly fits into the category of a mythical quest for the Holy Grail. Erythroblasts cultured in vitro from peripheral blood CD34+ progenitors are able to efficiently enucleate, producing reticulocytes that are phenotypically similar to donor-derived red cells. Rebecca McDonald and Cedric Ghevaert go on to describe RESTORE as the first-in-human crossover study investigating the survival of red cells derived in vitro compared to donor-derived red cells in the circulation using Cr51 labelling.
There are many potential and exciting applications of this technology. Genome editing may support the production of non-immunogenic ‘universal’ blood cells or blood cells negative for antigens that make transfusion of multi-alloimmunised patients highly difficult, and perhaps even HLA null platelets and platelets with enhanced haemostatic properties.
There are, however, huge challenges and many questions ahead. Nevertheless, the current stage where manufactured red cells are being transfused to humans as part of this study does represent ‘a triumph of science’, as stated by the authors.
They acknowledge the dedication and skills of a very large team and commitment by funders and organisations across the UK, paving the way for future trials with cellular therapies and manufactured advanced blood products.
The potential for using cellular immunotherapy, such as CAR-T cells, has significant hurdles to overcome...
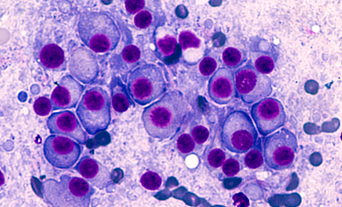
Novel treatments for multiple myeloma
Multiple myeloma is a malignant disease of plasma cells in the bone marrow with complex genetic heterogeneity. Delayed diagnosis is common and patients typically have a remitting and relapsing course with initial response often leading to resistant disease.
Guy Pratt’s thoughtful article starts off by highlighting many challenges, including late diagnosis, difficulties in criteria around initial intervention, assessing and interpreting minimal residual disease, and standards of supportive care. He goes on to cover exciting developments with the ‘explosion of newer treatments’ including immunomodulatory drugs, proteasome inhibitors and the more recent monoclonal antibodies targeting CD38 in plasma cells. The potential for using cellular immunotherapy, such as CAR-T cells, has significant hurdles to overcome, including high relapse rates, toxicity and cost. Treatments that are developed for specific genetic subtypes of myeloma are still in early development.
The article concludes by highlighting that myeloma is now one of the most expensive cancers to treat, with patients needing multiple lines of expensive agents and a potential gulf between what is licensed and what is affordable, as stated by agencies in the UK such as NICE and the Cancer Drugs Fund. There are ongoing significant challenges in the management of this disease, particularly in elderly and frail patients.
AMR is now the third-leading underlying cause of death globally...
The slow pandemic
Finally, we have included a transcript of the flagship Diamond Jubilee lecture ‘Antimicrobial resistance – the slow pandemic’ given in September 2022 at the UK Federation of Infection Societies meeting by Professor Dame Sally Davies, UK Antimicrobial Resistance (AMR) Special Envoy to the UN. New data confirms that AMR is now the third-leading underlying cause of death globally, with the most vulnerable bearing a disproportionate burden.
The WHO has highlighted the lack of treatments in development that will address critical public health needs and states that, consequently, "the world is failing on AMR". Policymakers, healthcare workers and the public can learn from the COVID-19 pandemic to increase innovation, access and stewardship of antimicrobial treatments globally, with attention needed to new solutions that are now being trialled across the world.
Meaningful progress in the science behind the cure
It was a pleasure to review the above expert articles, which highlight some excellent examples where real, meaningful progress has been made in understanding ‘the science behind the cure’ and embarking on the challenging journey to translate these discoveries into improvements in patient care.